In recent years, breakthroughs in genetics and DNA testing have revolutionised healthcare, especially in cancer diagnosis, treatment, and care. By examining a person’s genes, we can now identify people at higher risk of developing certain cancers.
This allows healthcare providers to detect cancers at an earlier stage and make informed decisions about cancer management and surveillance. Crucially, they can also offer more effective personalised treatments and prevention strategies based on the patient’s genetic profile.
Report found:
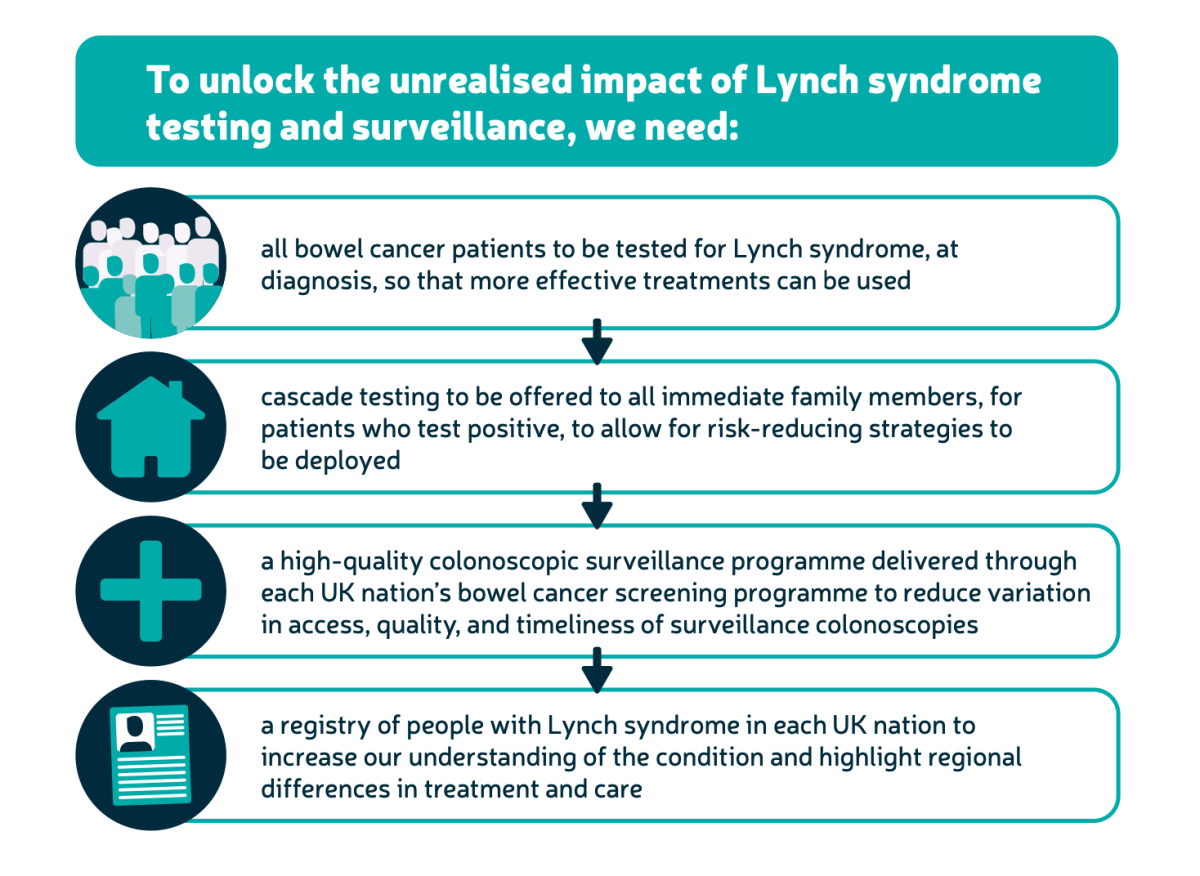
- There have been significant improvements in genetic testing for bowel cancer patients, with an average of 9 in 10 newly diagnosed bowel cancer patients being tested over the last financial year, but workforce and capacity issues are still barriers.
- Half of health authorities who responded, reported that family members of people with Lynch syndrome aren’t offered letters they can take to their GP, which is one route to accessing genetic counselling and testing.
- A postcode lottery for life-saving routine surveillance colonoscopies exists. Although surveillance is offered to all Lynch syndrome patients in England through the Bowel Cancer Screening Programme, only 6 in 10 health authorities across Scotland, Wales and Northern Ireland offer surveillance colonoscopies in line with clinical guidance.
- Major gaps in data collection and reporting on Lynch guidance and services are holding back Lynch syndrome care.
Testing all newly diagnosed bowel cancer patients for Lynch syndrome and implementing routine colonoscopic surveillance are crucial steps in meeting the early diagnosis goals set by governments and health services nationwide.