Thank you Patricia for devoting your valuable time to trying to improve the Situation in Ireland.
This is what Patricia wrote…..
Some of you may not like what I have to say here but those who met me will know I am always honest and frank in my views.
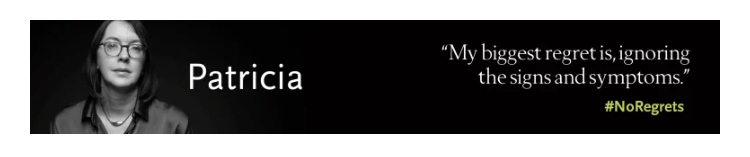
My advocacy work has been done as part of our Irish Colorectal Cancer Community but in this email I wanted to share my personal views. I am now at end of life and under the care of community palliative care. I was diagnosed 3 years ago (at 47 years of age) with metastatic colorectal cancer (early onset Colorectal Cancer: eoCRC) and I have been fortunate to have lived a good quality of life for 3 years on systemic treatment which allowed me to engage in advocacy.
Early-onset colorectal cancer (eoCRC)is colon cancer or rectal cancer diagnosed before the age of 50. The American Cancer Society says the incidence of eoCRC is expected to increase more than 140% by 2030. Watch this video to learn more: ASCO eoCRC Global Trends
I became an advocate for a number of reasons and the primary one was to try to improve outcomes for patients who come after me. I was shocked at how CRC in Ireland seemed to be ignored; I had previously had breast cancer and I couldn’t understand how little attention CRC received. It also gave me a purpose while living with my diagnosis as I was losing so many other parts of my life to this terrible disease.
Over the last 18 months as a patient advocate I looked to see how Ireland could improve the preventive and diagnostic pathways for patients so CRC is caught early. These improvements are too late for me but they are critical so that others can be diagnosed earlier. The priority changes I would want to see are:
- Access to diagnostics pathways to address the need of patients below 59 who are not met by the poor Bowel screening programme in Ireland
- Better education and awareness with GPs so symptomatic patients are not dismissed as being too young with the rise of Early Onset Colorectal Cancer
- Guidelines and diagnostic options for GPs (GP Guidelines) that reflect the rise of Colorectal Cancer (CRC) in people under the screening age
I know how long it takes to implement changes in Ireland and I could see our nearest neighbours updating their guidelines to reflect the new needs. I attended the Bowel Cancer UK event in Stormont to hear what the new diagnostic pathways being implemented there and I watched as the US and Australia dropped screening ages to 45. On #medtwitter I was seeing researchers, medics and charities talking about this – but where were the people in Ireland?
I expected funds and resources would be invested in the prevention and early diagnosis of CRC – it can be found as polyps even before cancer develops and all economic models support earlier screening. There must be lots of research and investment in this area – right?
- I assumed someone must be doing something out there for the 2,562 patients diagnosed each year with 1,001 deaths per annum (female 423, male 579).
- There is a bowel screening programme so surely more can be done for these patients – the screening programme is way behind global leading practice and people are being diagnosed too late and dying as a result.
- Based on the available NCRI data (2018-2020.), there are more CRC deaths per annum (1,001) than the combined deaths from the other 2 screening programmes – cervical (89) and breast cancer (748).
- I feel that one consequence of the cervical cancer scandal is that other screening programmes, especially Bowel, are not prioritised and there is a fear of change. 5 times morewomen die of CRC (423) each year than cervical cancer (89). If you follow @hseNCCP and @NSShse on Twitter you think they only cover Cervical Cancer.
I started reaching out and began with the Irish Cancer Society – I assumed our primary cancer charity, with a research arm, would be focusing on working with their partners to ensure our health guidelines and policy were being prioritized in line with what I was seeing happening in other western countries. When we spoke of eoCRC it was the first time they even seemed to know this was something worth thinking about and I see no pro-active engagement. I expect they will reach out soon for the mandatory patient stories and photo ops for April’s Bowel Cancer Awareness month.
I also met with the NCCP to present our priorities, a meeting that took 3 months to arrange and for which I had spent precious days and weeks preparing the priorities. The meeting opened with the NCCP saying they have no agenda, no one bothered to read what was sent, our views and opinions were dismissed. I personally have never felt so angry in my professional career about the way I and my fellow advocates on the call were treated. CRC (Bowel Cancer) GP guidelines and prevention are not a priority for the NCCP. If I look at the NCCP board minutes. CRC (Bowel Cancer) is barely mentioned apart from Bowel Screening update figures as an FYI. I asked about the Endoscopy Working Committee and their recommendations, I received no information and it appears that they do not currently meet. NCCP colleagues declined the invitation to attend the seminar (Let’s Talk about Colorectal Cancer) last year. I guess no one wants a spotlight on these blind spots and gaps. Based on where things are now it will be at least 2027/2028 before any change could be implemented and this is only if it actually makes the list of things to look at.
For politicians, the answers to any parliamentary questions clearly show the lack of any urgency to reassess the current strategy. The question you need to ask is how we are catching the disease in the under 59s? Would this level of deflection and delay be accepted for Breast Cancer patients? Imagine the Joe Duffy Liveline calls.
Within the Research Community I was assuming that with all the millions of euros spent in Ireland across the charity, university and hospital networks I would find people who were working on research that would make sure Irish CRC patients are not left behind. But I guess that is where I was further disappointed. There is so much PR around research in Ireland, photo shoots, poster presentations, PPI awards. This is a small country, all highly connected and networked but it feels like a world of silos and individual and institutional priorities – not the priorities of the Irish public and patients who fund much of this.
After reflecting on my meetings, chats, interactions and conferences there are a number of areas of research I was would like you to reflect on:
- What is the last research project that improved the outcome for any significant cohort of patients in Ireland, specifically a CRC patient?
- Why is there no research funding in Ireland addressing preventive and pragmatic topics that can actually be implemented for the population?
- Where is the medical community – surgeons, GPs, oncologists – who should be shouting for changes as they see their waiting rooms fill up with more and more younger patients?
- What happens to the research from Health Economists that show the cost effectiveness of better screening programmes? I’ve seen the presentations but who does anything with this?
- Why is so much focus on research on medical oncology drugs where the international and commercial community are already spending billions? We are wasting money and time repeating research already done.
I will end where I should have started – the Patient.
My question on patient involvement is why do you want it in the first place? My experience is that it looks good for photos, funding and PR but considering the type of research being undertaken, there is often actually little value for either party and just a waste of energy. And if it is that important, then here are my experiences and why I would not be supporting research unless theses issues are addressed:
- Patient views dismissed when not in line with the research or policy idea – what is the point of getting patient input when the research idea is already defined?
- My experience is that researchers have very little knowledge about the disease and the patient’s lived experience, making incorrect assumptions and they do not know how to engage with patients. For example, a researcher asked for my input in his final funding stage – my feedback was dismissed when I challenged some aspects. My experience as a patient with 2 years on different treatments was refuted.
- There is no standard PPI engagement model, no defined way of working with patients or compensating them. I was often the only person not being paid for my contribution. It is left to each researcher or function to figure it out. Patients are often not compensated at all, and definitely not for travel expenses to participate in events they are asked to join, do your staff get paid taxi and train fares when needed? You do realise you automatically exclude patients who may have lost their income and cannot afford to participate. The All4One vouchers I received recently as compensation are not accepted by the funeral directors I was meeting that afternoon.
I’ve had good experiences over this time that give hope. The amazing commitment from the Marie Keating Foundation. The recent establishment of the RSCI PriCAN centre, though this needs to be expanded to CRC. And finally, I hope to see the results of the Cancer Trials Ireland patient-led survey to understand the experience of living with metastatic breast cancer. Recommendations must be implemented for all cancers, not only breast cancer patients, the experiences are the same.
In summary, the Irish health system is failing patients to prioritise early diagnosis and is not prepared for the rise in eoCRC in the coming years.
I am sure some of you may dispute what I have written but this is my experience and I believe it is important to get these words on a page and share with this community. I want to thank all of you who were generous with your time and insights and I know that some on this email will agree with many of my points.
Be mindful and respectful of patients, don’t just use them for funding approvals and photo opportunities.
I ask that you consider what I have said, assess your organisations’ commitment to CRC and prioritise prevention and early detection of CRC and save hundreds of lives. This is one of the cancers that can be found at a pre-cancerous polyp stage.
Finally, please support the Marie Keating Colorectal/ Bowel Cancer Awareness Call to Action campaign that will launch in April. You might see or hear from me again there.
Thank you for reading to the end.
Patricia