According to the European Hereditary Tumour Group’s latest position report, LS is now considered an umbrella term for four distinct types of LS: MLH1 syndrome, MSH2syndrome, MSH6 syndrome, and PMS2 syndrome. These syndromes vary with regard to the age of onset of the associated cancers, sex predominance, and cancer incidence rates.
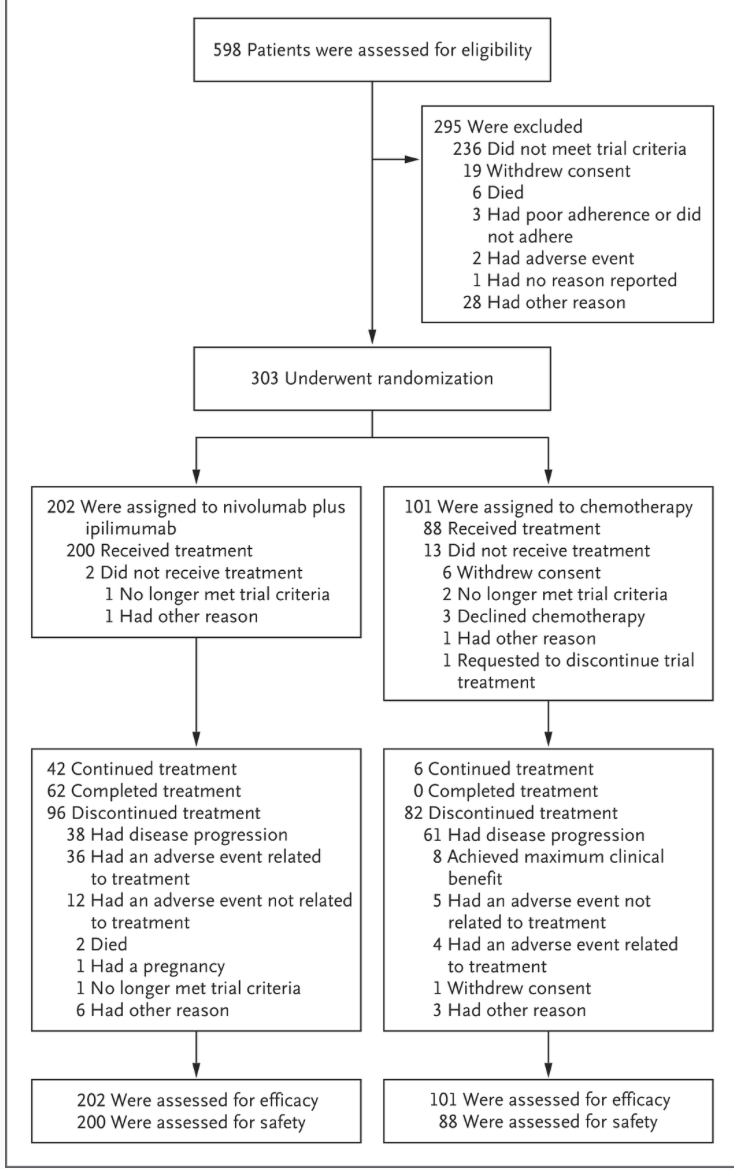
Numerous retrospective studies and several meta-analyses support the increased risk of metachronous CRC, despite segmental resection, recommendations for extended resection remain a subject of debate due to the current absence of prospective studies and randomised trials.
Furthermore, no survival benefit has been demonstrated for extended surgery. A quality-of-life comparison between patients who had undergone segmental resection and patients who had undergone subtotal colectomy did not find a significant difference, but the latter group had poorer functional outcomes
https://academic.oup.com/bjs/article/112/4/znaf061/8113421#google_vignette