Dr Kai-keen Shiu LS Annual Conference 2025
Category: Research
Dr Kevin Monahan-Lynch Syndrome UK Annual Conference 2025
Lynch Syndrome where we were and where we are now.
Hereditary Cancer Syndrome Carriers: Feeling Left in the Corner
Objectives: There is limited evidence on health promotion interventions in people with hereditary cancer syndromes or on their main sources of support and information. This study aimed to understand these patients’ experiences and needs, including their information needs, their views on prevention and mental health, and the support they want from nurses. (small study)
Conclusions: People with hereditary cancer syndromes need professionals to be involved in their long-term management and to provide reliable information. As genomics are increasingly integrated in oncology, the need for professionals to support these populations will increase.
Implications for nursing practice: Nurses are crucial for promoting self-management and advocating for patient decision-making; however, they need skills and knowledge to do so. There is a need for nurses to get more involved in understanding hereditary cancer syndromes and an opportunity to take the lead in the care of these people.
The Cancer Prevention Project 3 study (CaPP3)
The trial involved 1,879 people with Lynch syndrome who were given three different-sized doses of the painkiller.
The Cancer Prevention Project 3 study (CaPP3), supported by Cancer Research UK, involved patients taking a different daily dose of aspirin: 100mg, 300mg or 600mg. In the trial, a European-sized dose of 100 mg aspirin was used. The established dose is 75mg per day in the UK, and 81mg in the US.
People with Lynch syndrome have inherited a faulty gene which can increase their chances of developing some cancers – including bowel and womb cancer.
Prof John Burn, who led the international study, said he focused his research on those patients “because they get so many cancers”.
“We already have NICE guidance saying people with Lynch syndrome should be recommended to take aspirin. Now we should recommend a baby aspirin.” new results showed the lowest dose worked just as well as the larger doses.
“Roughly speaking, if someone with Lynch syndrome has about a 2% a year chance of getting mostly bowel cancers, we think if they take aspirin, that is halved – down to about 1% a year,” he explained.
In some people, aspirin can cause bleeding, so Prof Burn said he wanted health regulators to now recommend the lowest dose be given to Lynch syndrome patients.
Nonoperative Management of Mismatch Repair–Deficient Tumours
Among patients with mismatch repair–deficient (dMMR), locally advanced rectal cancer, neoadjuvant checkpoint blockade eliminated the need for surgery in a high proportion of patients. Whether this approach can be extended to all early-stage dMMR solid tumours, regardless of tumour site, is unknown.
A total of 117 patients were included in the analysis. Phase 2 study.
CONCLUSIONS
Among patients with early-stage dMMR solid tumours that were amenable to curative-intent surgery, neoadjuvant PD-1 blockade led to organ preservation in a high proportion of patients.
https://www.nejm.org/doi/full/10.1056/NEJMoa2404512?query=WB
Clinical referral to the NHS following multi-cancer early detection test results from the NHS-Galleri trial
The large, randomised, controlled NHS-Galleri trial (NCT05611632) is assessing the clinical utility of a multi-cancer early detection (MCED) test for asymptomatic cancer screening in England.
Conclusions: To our knowledge, the NHS-Galleri trial has established the first model for the standardised clinical referral of asymptomatic individuals from a trial into NHS standard-of-care cancer pathways. We hope insights from our work could help accelerate screening trial conduct in the UK, and support MCED population screening programme implementation in future.
https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1511816/full
The Myth that Cervical Screening Checks for All Gynecological Cancers
Research in Ireland commissioned by the Irish Network of Gynaecological Oncology (INGO) and supported by Breakthrough Cancer Research highlights the misconceptions that exist surrounding cervical screening, showing that one in three women in Ireland (34%) mistakenly believe that cervical screening checks for all five gynecological cancers
(https://isgo.ie/ingo-outputs/).
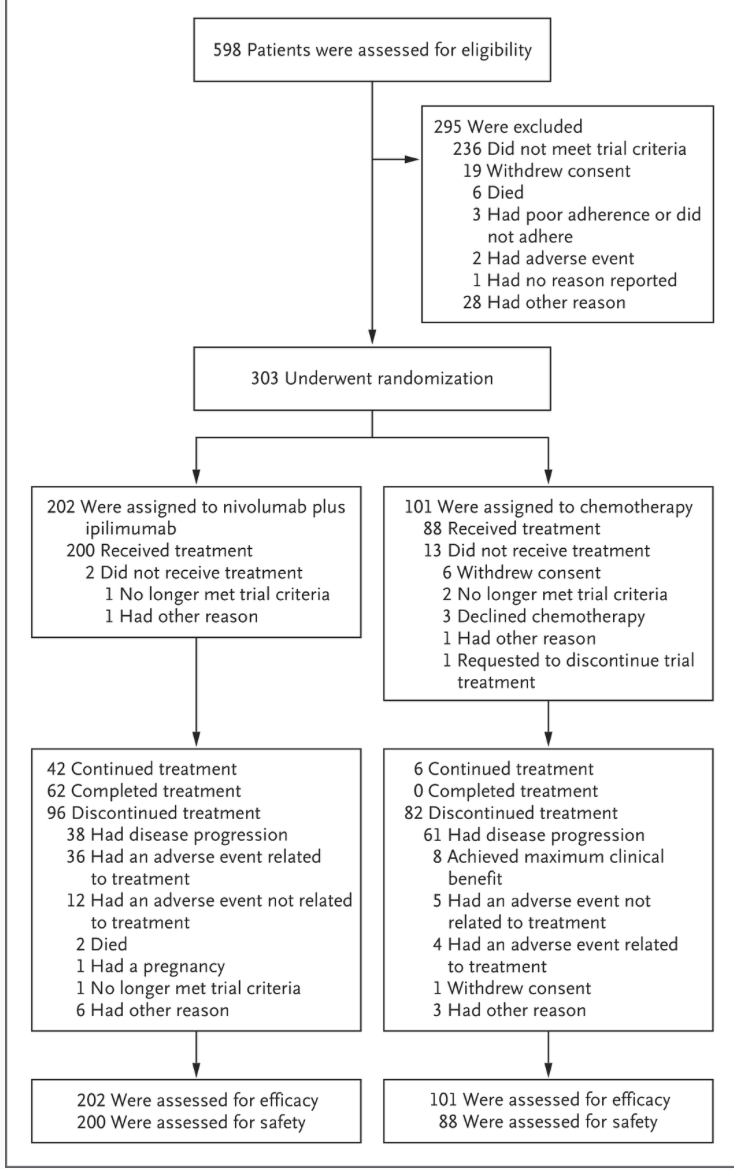
Nivolumab plus Ipilimumab in Microsatellite-Instability–High Metastatic Colorectal Cancer
In this phase 3, multinational, randomised trial, , progression-free survival outcomes with nivolumab plus ipilimumab were superior to those with chemotherapy in the first-line treatment of MSI-H or dMMR metastatic colorectal cancer.
Grade 3 and 4 treatment-related toxic effects were consistent with the established profiles of each individual drug, and no new safety concerns were identified.
Improving Cancer Outcomes with Better Lynch Syndrome Testing: A Cost-Benefit Study
While testing of colorectal cancer tumours for mismatch repair defects has been recommended for years, the majority of patients with abnormal results do not complete the next steps, including genetic testing.
Completed genetic testing would determine whether a patient had Lynch syndrome (LS), a hereditary marker for a higher-than-average predisposition for developing colorectal cancer as well as other cancers, including endometrial and ovarian. Early identification of LS in a patient’s family members has the potential to reduce their cancer risk and mortality, increasing the medical benefit of and thereby ultimately lowering testing costs, the study found.
Metachronous colorectal cancer risks after extended or segmental resection in MLH1, MSH2, and MSH6 Lynch syndrome: multicentre study from the Prospective Lynch Syndrome Database
According to the European Hereditary Tumour Group’s latest position report, LS is now considered an umbrella term for four distinct types of LS: MLH1 syndrome, MSH2syndrome, MSH6 syndrome, and PMS2 syndrome. These syndromes vary with regard to the age of onset of the associated cancers, sex predominance, and cancer incidence rates.
Numerous retrospective studies and several meta-analyses support the increased risk of metachronous CRC, despite segmental resection, recommendations for extended resection remain a subject of debate due to the current absence of prospective studies and randomised trials.
Furthermore, no survival benefit has been demonstrated for extended surgery. A quality-of-life comparison between patients who had undergone segmental resection and patients who had undergone subtotal colectomy did not find a significant difference, but the latter group had poorer functional outcomes
https://academic.oup.com/bjs/article/112/4/znaf061/8113421#google_vignette