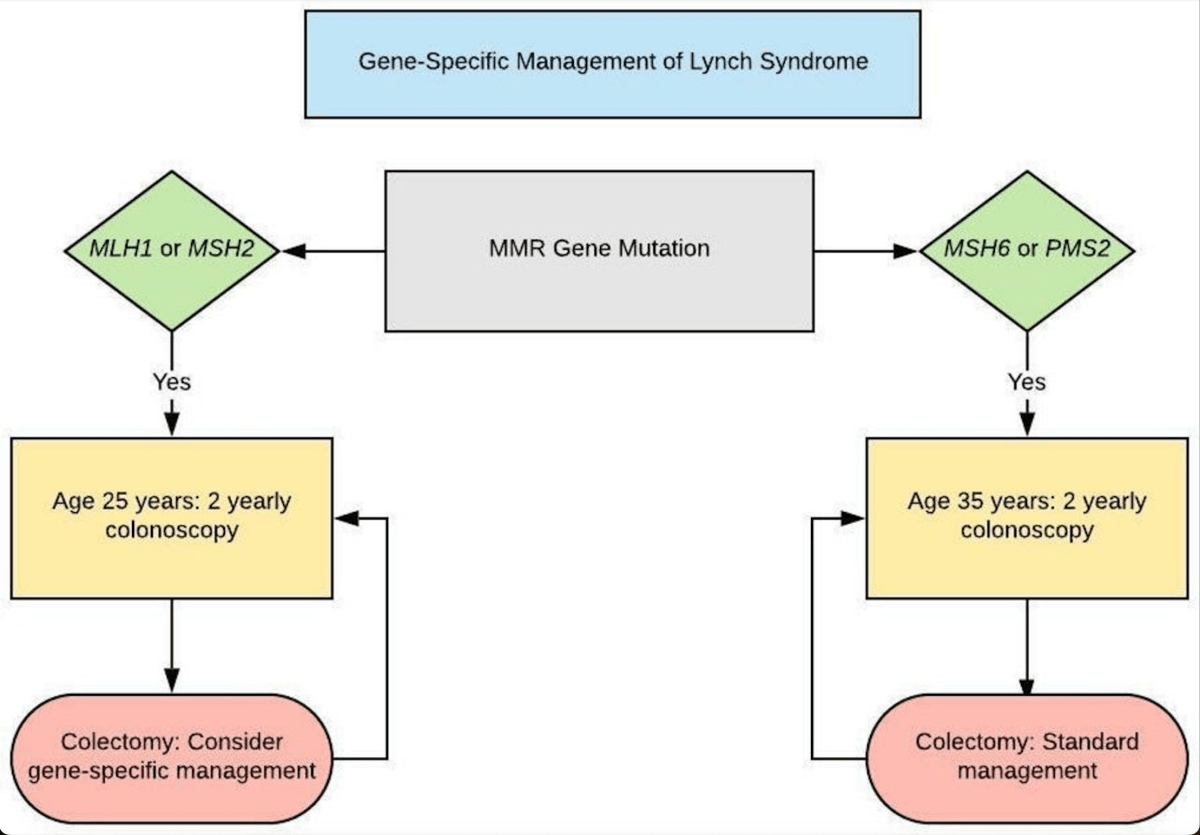
Discoveries enabled better understanding of how the DNA mismatch repair (MMR) system not only recognises DNA damage but also responds to damage by DNA repair or by triggering apoptosis(cell death) in the injured cell.
What has happened over the past 37 years was not predictable when this journey began, but it does speak to the power of careful scientific experimentation, following the facts, perseverance in the face of opposition, and the willingness to think outside of established paradigms.
The conclusion that CRCs with MSI responded differently to classical cytotoxic chemotherapy than did non-MSI CRCs and eventually, the key clinical paradigm shift was the discovery of ICT(Immune checkpoint therapy and its unique effect on tumours with MSI.
Some of these concepts required brilliant thinking and interpretation and others seemingly announced themselves after the correct understanding of an unexpected observation. Since this astonishing series of events unfolded over about four decades, there is hope that this remarkable progress will continue into the future.
https://link.springer.com/article/10.1007/s10620-023-08006-z#Sec18