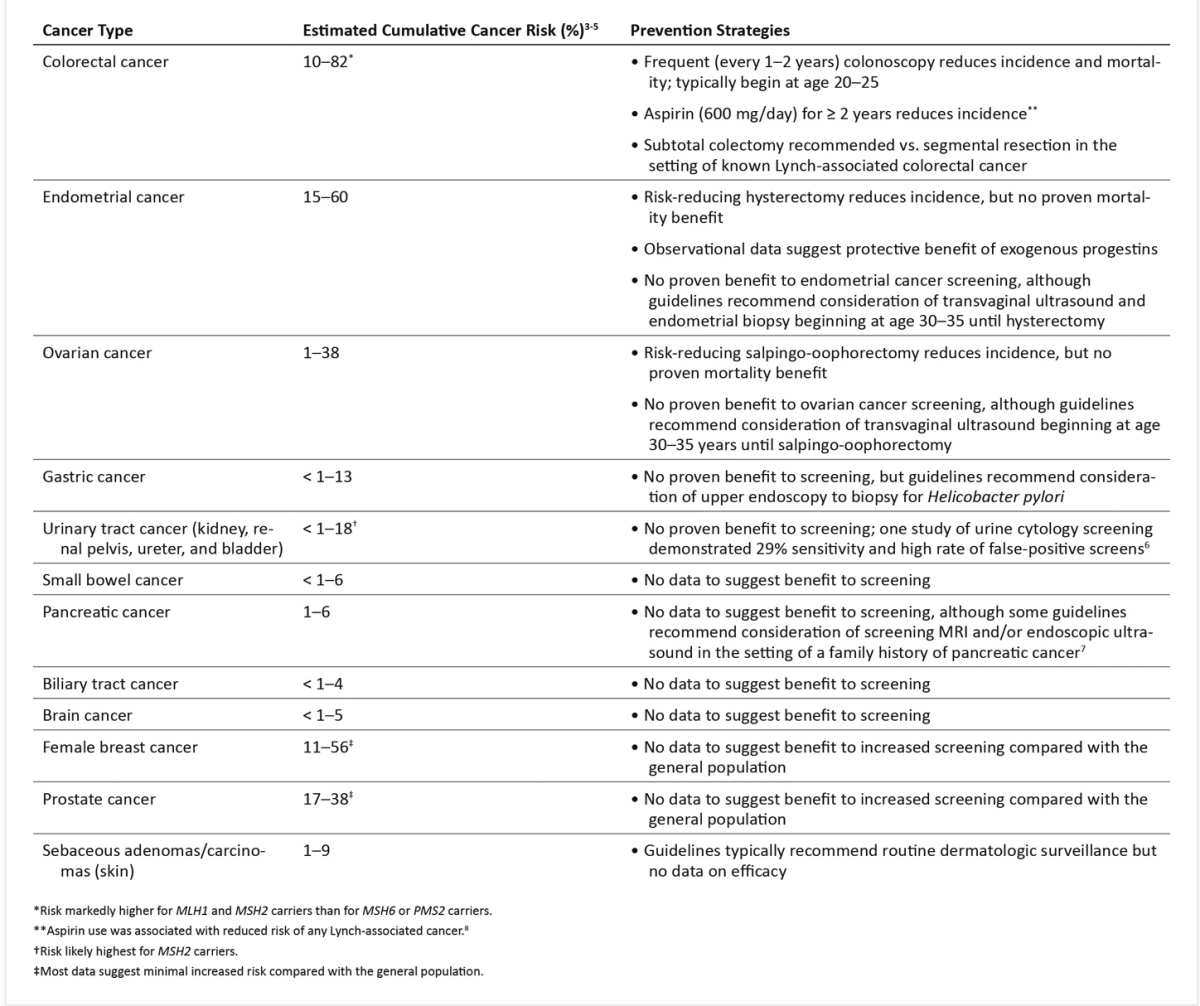
Lynch syndrome may affect up to 175,000 people in the UK and is linked to 3% of cases of womb cancer. To develop Lynch syndrome, you need to have one parent that carries the gene. Someone diagnosed with Lynch syndrome has up to 60% chance of developing womb cancer in their lifetime. Lynch syndrome is also associated with an increased risk of bowel cancer. Those diagnosed with Lynch syndrome undergo regular tests to check for bowel cancer and womb cancer, many will be offered a hysterectomy (operation to remove the womb) to prevent womb cancer once they feel their family is complete.
Lynch syndrome is often diagnosed when a strong family history of bowel or womb cancer is noted. If you feel this may apply to you, please speak to your doctor about being referred to a genetics service. More information on Lynch syndrome can be found here.
https://peachestrust.org/womb-cancer/risk-factors-prevention/