Hereditary factors play a key role in the risk of developing several cancers. Identification of a germline predisposition can have important implications for treatment decisions, risk-reducing interventions, cancer screening, and germline testing.
Key Points:
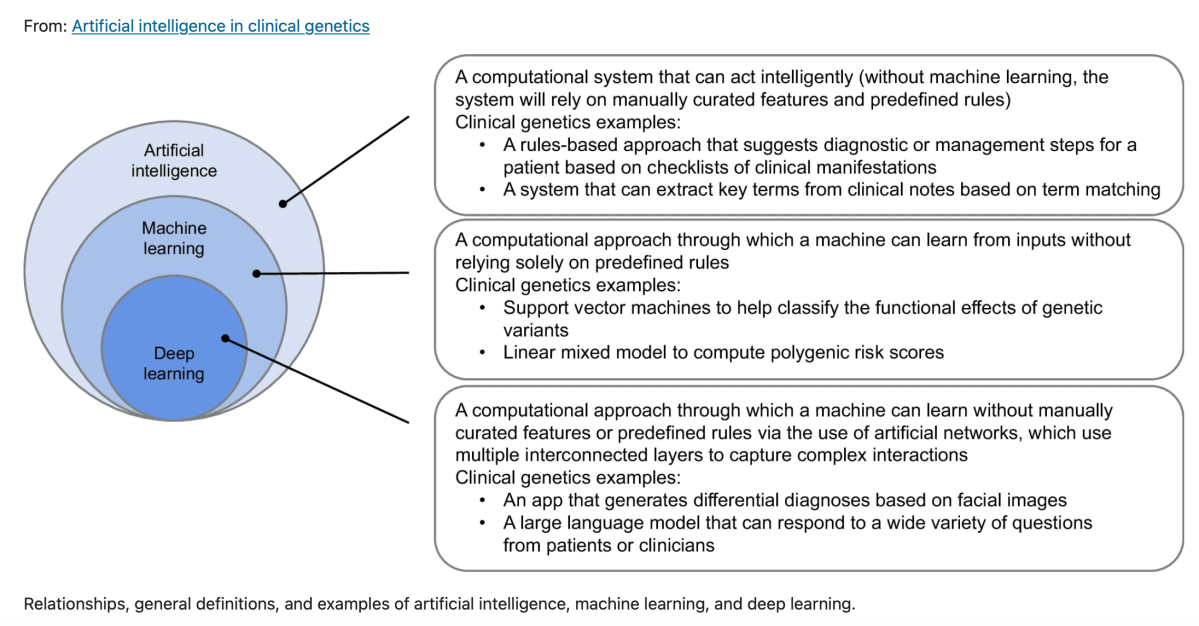
Questions Does universal genetic testing in patients with cancer identify more inherited cancer predisposition variants than a guideline-based approach, and what is the association between universal genetic testing and clinical management?
Findings In this multicenter cohort study of 2984 patients with cancer, 1 in 8 patients had a pathogenic germline variant, half of which would not have been detected using a guideline-based approach. Nearly 30% of patients with a high-penetrance variant had modifications in their treatment based on the finding.
Meaning Universal genetic testing detected more clinically actionable variants than a guideline-based approach, with a significant association with clinical management for the patients and their families.
https://jamanetwork.com/journals/jamaoncology/fullarticle/2772576/