Conclusion:
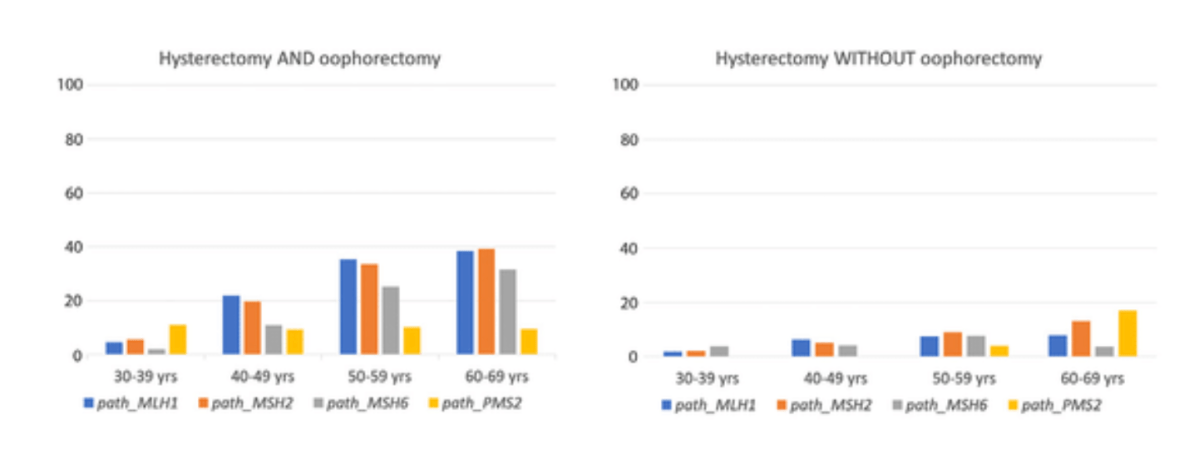
Uptake of RRS before 50 years of age was low, and RRS was rarely undertaken in association with surgical treatment of CRC.
Uptake of RRS aligned poorly with gene- and age-associated risk estimates for endometrial or ovarian cancer that were published recently from PLSD and did not correspond well with current clinical guidelines.
The reasons should be clarified. Decision-making on opting for or against RRS and its timing should be better aligned with predicted risk and mortality for endometrial and ovarian cancer in Lynch syndrome to improve outcomes.