“In navigating the effects of accelerated aging post-oophorectomy, HRT can be an essential tool for those who have not achieved menopause. While it can alleviate various symptoms and health risks, it is crucial to discuss its potential benefits and drawbacks with a healthcare provider.”
Category: Monitoring
Exploring Stakeholders’ Perspectives on Implementing Universal Germline Testing for Colorectal Cancer: Findings From a Clinical Practice Survey
CONCLUSION: This study(Eighty CGA-IGC members participated) demonstrates wide support among hereditary GI cancer experts for implementation of UGT for patients with CRC. However, alternative service delivery models using nongenetics providers should be considered to address the logistical barriers to UGT implementation, particularly the growing demand for genetic testing.
In conclusion, there is broad support for UGT for all newly diagnosed patients with CRC among the members of the CGA-IGC.
However, changes to practice, such as alternative service delivery models or standardization of test choice, will likely have to be implemented to meet the increased patient volume.
Additional studies are needed to compare UGT implementation strategies (eg, traditional or alternative service delivery models) to ensure there is equitable access to genetic testing and improved outcomes for patients with CRC.
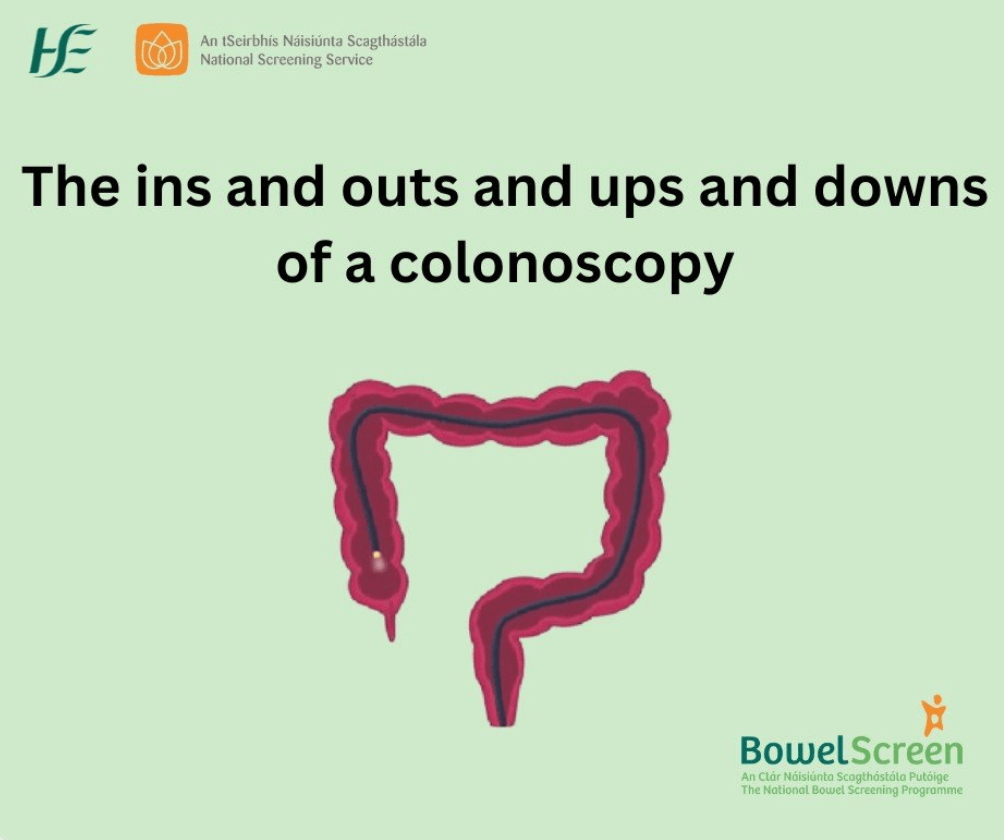
The ins and outs and ups and downs of a colonoscopy
So what is a colonoscopy?
A colonoscopy is a test to look at your bowel using a small camera. The test looks for any small growths called polyps, or signs of disease, such as bowel cancer. If polyps are found they are usually removed during the test. This will reduce the risk of cancer developing. If they are not removed they might turn into cancer. If bowel cancer is found early, it’s easier to treat and there’s a better chance of recovery.
Genetic testing and the future of medicine
More common signs of hereditary cancer include:
- Multiple cases of cancer on the same side of the family, especially breast, colorectal, endometrial or ovarian cancers.
- Cancer diagnosed before age 50, especially breast, colorectal or endometrial.
- Rare cancers at any age, including:
- ovarian
- pancreatic
- male breast
- metastatic prostate
The future of genetic testing
Dr. Steiner is optimistic about the future of genetic testing and how it can impact healthcare care. “I think in the not-too-distant future, everybody will have comprehensive genetic testing done in order to prepare healthcare providers for any future issues a patient might develop.”
When that happens, genetic testing will be used more often to help people and their healthcare providers prevent unexpected diagnoses.
https://www.facingourrisk.org/XRAY/genetic-testing-and-future-of-medicine
The English National Lynch Syndrome transformation project: an NHS Genomic Medicine Service Alliance (GMSA) programme
Conclusion: This ongoing transformational project is strongly supported by stakeholders in England. Significant quality improvement has been implemented, facilitating systematic delivery of universal testing for LS nationally and reduction in variation in care.
“Only by ‘mainstreaming’ of genetic testing by the same cancer multidisciplinary teams that diagnose and treat cancer locally can we ever hope to effectively find diagnoses of Lynch syndrome and open up the door to better cancer prevention survival” Kevin Monaghan(Gastroenterologist from @StMarksGenomics)
Novel Stool RNA Test More Sensitive for Detecting Colon Cancer Versus FIT
The novel multitarget stool RNA test (ColoSense) showed high sensitivity for detecting colorectal neoplasia(new, uncontrolled growth of cells) among adults ages 45 and older, according to the phase III prospective CRC-PREVENT trial.
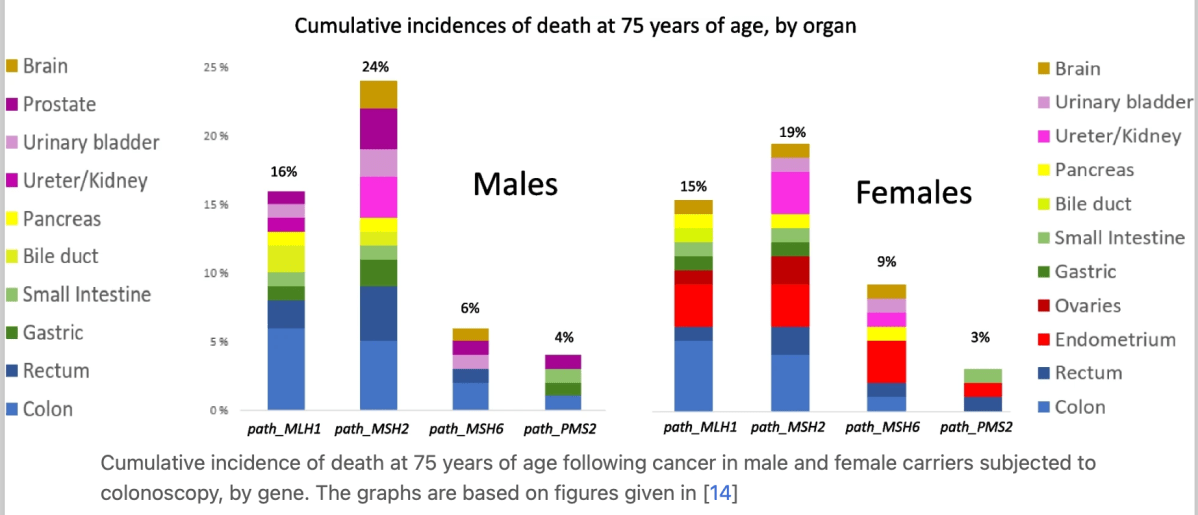
Dominantly inherited micro-satellite instable cancer – the four Lynch syndromes – an EHTG, PLSD position statement
Improved survival following early diagnosis and treatment of MSI cancers of the colon, endometrium and ovary has led to carriers living on and contracting subsequent cancers in other organs. These have worse prognoses.
Tests for MSI have generally been optimised to demonstrate MSI colon cancers, but the different Lynch syndrome genes have different organ specific penetrance and expressivities. The prevalence of MSI in cancers in these other organs is not well studied, with respect to either how to test for MSI cancers in these organs or to estimate the frequency of MSI cancers. Identifying such MSI cancers would be of interest to select cases for immunotherapy tailored against MSI cancers.
The obvious next steps for clinical research on the MSH2 and MLH1 syndromes include determining the effects of immunotherapy for cancers with currently poor prognoses.
https://hccpjournal.biomedcentral.com/articles/10.1186/s13053-023-00263-3
NCCN guidelines
Genetic/Familial High-Risk Assessment: Colorectal
- NCCN Guidelines Version 1.2023
– Adenomatous Polyposis Testing Criteria
– Attenuated Familial Adenomatous Polyposis
– Colonic Adenomatous Polyposis of Unknown Etiology
– Familial Adenomatous Polyposis
– Juvenile Polyposis Syndrome
– Lynch Syndrome
– MUTYH-Associated Polyposis
– Peutz-Jeghers Syndrome
– Serrated Polyposis Syndrome
When Your Family Is Impacted by Hereditary Cancer – An Interview with My Sister
Cancer is scary and heredity (not just BRCA mutations) plays a huge role in some families.
Launch of Hereditary Cancer Model of Care (Ireland)
Hereditary Cancer Model of Care provides the blueprint for the necessary development of services for the identification and management of people with an inherited cancer predisposition (e.g. Lynch syndrome or BRCA gene cancer risk), in order to harness the power of genetics to reduce cancer risk, and improve patient outcomes and quality of life.
The model of care will ensure/support the development of:
- Development of national guidance to underpin standardised best practice, including mainstreaming of cancer genetic testing
- Equitable access to hereditary cancer services for all
- Clear governance and clarity regarding the roles of national genetics and genomic structures, specialist cancer genetics services and regional cancer predisposition services, within an overarching model of care
- Commitment to the Sláintecare principles of right person, right place, right time – through the integration of genetic assessment and testing into regional services, with access to specialist genetic expertise as required
- Maximal use of technological solutions
- Timely access to genetics assessment and testing, including specialist cancer genetics expertise as required
- Timely access to clinical management of cancer predisposition, including risk reduction options
- Comprehensive and coordinated approaches to ongoing management
- Quality assurance of service
- Access to high quality patient information, psychological support and peer support for patients
- Education and training of health care professionals, including accredited training for those delivering mainstreamed pathways