The novel multitarget stool RNA test (ColoSense) showed high sensitivity for detecting colorectal neoplasia(new, uncontrolled growth of cells) among adults ages 45 and older, according to the phase III prospective CRC-PREVENT trial.
Category: Prevention
Dominantly inherited micro-satellite instable cancer – the four Lynch syndromes – an EHTG, PLSD position statement
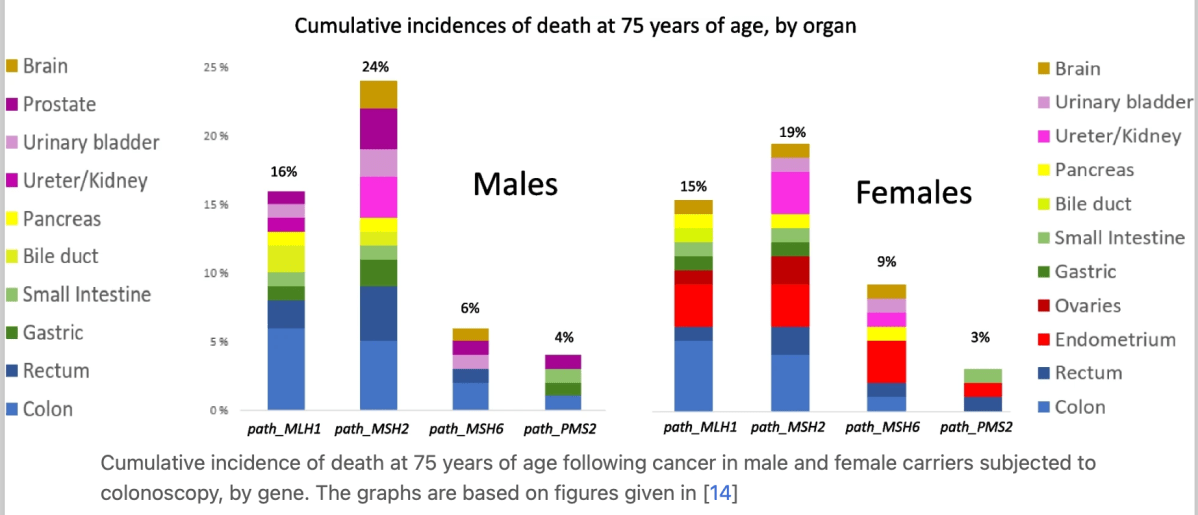
Improved survival following early diagnosis and treatment of MSI cancers of the colon, endometrium and ovary has led to carriers living on and contracting subsequent cancers in other organs. These have worse prognoses.
Tests for MSI have generally been optimised to demonstrate MSI colon cancers, but the different Lynch syndrome genes have different organ specific penetrance and expressivities. The prevalence of MSI in cancers in these other organs is not well studied, with respect to either how to test for MSI cancers in these organs or to estimate the frequency of MSI cancers. Identifying such MSI cancers would be of interest to select cases for immunotherapy tailored against MSI cancers.
The obvious next steps for clinical research on the MSH2 and MLH1 syndromes include determining the effects of immunotherapy for cancers with currently poor prognoses.
https://hccpjournal.biomedcentral.com/articles/10.1186/s13053-023-00263-3
NCCN guidelines
Genetic/Familial High-Risk Assessment: Colorectal
- NCCN Guidelines Version 1.2023
– Adenomatous Polyposis Testing Criteria
– Attenuated Familial Adenomatous Polyposis
– Colonic Adenomatous Polyposis of Unknown Etiology
– Familial Adenomatous Polyposis
– Juvenile Polyposis Syndrome
– Lynch Syndrome
– MUTYH-Associated Polyposis
– Peutz-Jeghers Syndrome
– Serrated Polyposis Syndrome
When Your Family Is Impacted by Hereditary Cancer – An Interview with My Sister
Cancer is scary and heredity (not just BRCA mutations) plays a huge role in some families.
Why prevention is better than treatment for any gynecological cancer
Launch of Hereditary Cancer Model of Care (Ireland)
Hereditary Cancer Model of Care provides the blueprint for the necessary development of services for the identification and management of people with an inherited cancer predisposition (e.g. Lynch syndrome or BRCA gene cancer risk), in order to harness the power of genetics to reduce cancer risk, and improve patient outcomes and quality of life.
The model of care will ensure/support the development of:
- Development of national guidance to underpin standardised best practice, including mainstreaming of cancer genetic testing
- Equitable access to hereditary cancer services for all
- Clear governance and clarity regarding the roles of national genetics and genomic structures, specialist cancer genetics services and regional cancer predisposition services, within an overarching model of care
- Commitment to the Sláintecare principles of right person, right place, right time – through the integration of genetic assessment and testing into regional services, with access to specialist genetic expertise as required
- Maximal use of technological solutions
- Timely access to genetics assessment and testing, including specialist cancer genetics expertise as required
- Timely access to clinical management of cancer predisposition, including risk reduction options
- Comprehensive and coordinated approaches to ongoing management
- Quality assurance of service
- Access to high quality patient information, psychological support and peer support for patients
- Education and training of health care professionals, including accredited training for those delivering mainstreamed pathways
Fallopian Tubes and Ovarian Cancer: What’s the Connection?
Ovarian cancer almost always starts in the fallopian tubes.
Why is it called ovarian cancer if it doesn’t start there? For a long time, the ovaries were assumed to be the source because that is where the cancer is concentrated at the time of diagnosis.
Who should consider the procedure?
Women who have an average risk of ovarian cancer who no longer desire fertility but also want to reduce the risk of developing ovarian cancer might consider the procedure. Women with an elevated risk due to a gene mutation or family history should speak to their genetic counselor or doctor for more information.
What are the benefits and drawbacks?
For women with an average risk of ovarian cancer, the surgery has the potential to reduce the likelihood of ovarian cancer. The surgery is not reversible and causes infertility. Pregnancy is still possible, though only via in-vitro fertilization. For pre-menopausal women, removal of the fallopian tubes only, and not the ovaries, does not induce menopause.
The recovery time for fallopian tube removal is a few days to a few weeks, though the overall recovery time will depend on the primary reason for surgery.
A Guide to Lynch Syndrome
Lynch Syndrome is an inherited condition that increases your risk of developing some cancers, including bowel, womb and ovarian cancer. This is a guide to run through everything you need to know about Lynch.
This guide has been made with input from experts, people with Lynch Syndrome and Ask Eve nurses to provide you with all the information you need when offered testing for, or navigating a diagnosis of, Lynch Syndrome.
We also have an Easy Read guide to Lynch Syndrome, which you can download here
Philadelphia Girl, 14, Battling Three Cancers Simultaneously Hoping For a Breakthrough— The Rare Genetic Disorder Involved — How To Screen
Discovering that you or a family member have Lynch syndrome, Li-Fraumeni syndrome, or the BRCA1 and BRCA2 gene mutation, which increases the risk of developing breast and ovarian cancer, can be life-saving.
https://www.survivornet.com/articles/li-fraumeni-syndrome-importance-genetic-testing-sarcomas/
Why do we need to know if your cancer is hereditary?
If you find out your cancer is hereditary, knowing which gene mutations are involved enables you to:
• tailor your cancer treatments to your particular cancer, when possible;
• take available steps to decrease your risk of developing other cancers; and
• help your family members minimize their risk of cancer.
What if you don’t want to know?
Part of you may not want to know if your cancer is hereditary. Listen to the part of you that wants to do the best thing for your health and for your family. Finding out you have a mutation can be upsetting. Yet many patients report feeling relief and a renewed sense of control: “Learning I have a mutation does not change what is. It changes what I can do about what is.”