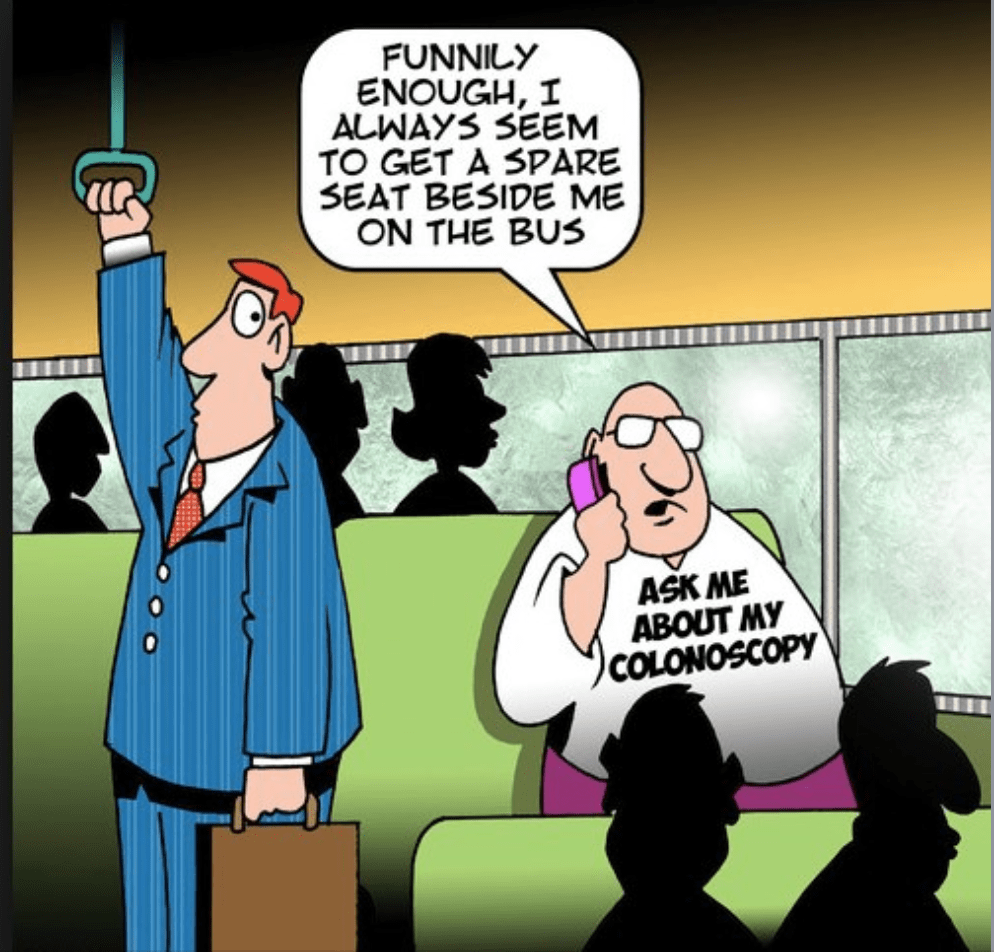
A colonoscopy is a test to look at your bowel using a small camera.
Bowel preparation is required by taking a strong laxative. You will take this the day before the test to empty your bowel. The test works best when your bowel is empty and there is nothing to block the camera going into the bowel and having a look.
You will have to go to a hospital endoscopy unit to have the test.
The test is a day procedure.
The test is done by a doctor or an advanced practice nurse, called an endoscopist.
You will have a choice of doing the test with sedation or no sedation.
Generally the test can take up to 20 minutes.
Before you leave, you will be told what was seen during the test and if any samples were taken or if any polyps were removed.
(Personally I have undergone aprox 15 colonoscopies and I can say that the preparation and procedure are worthwhile particularly if you have a family predisposition to cancer or have symptoms like blood in your stool. They have probably saved my life as during one of these procedures cancer was detected…I had no symptoms).
https://www2.healthservice.hse.ie/organisation/nss/news/the-ins-and-outs-and-ups-and-downs-of-a-colonoscopy/