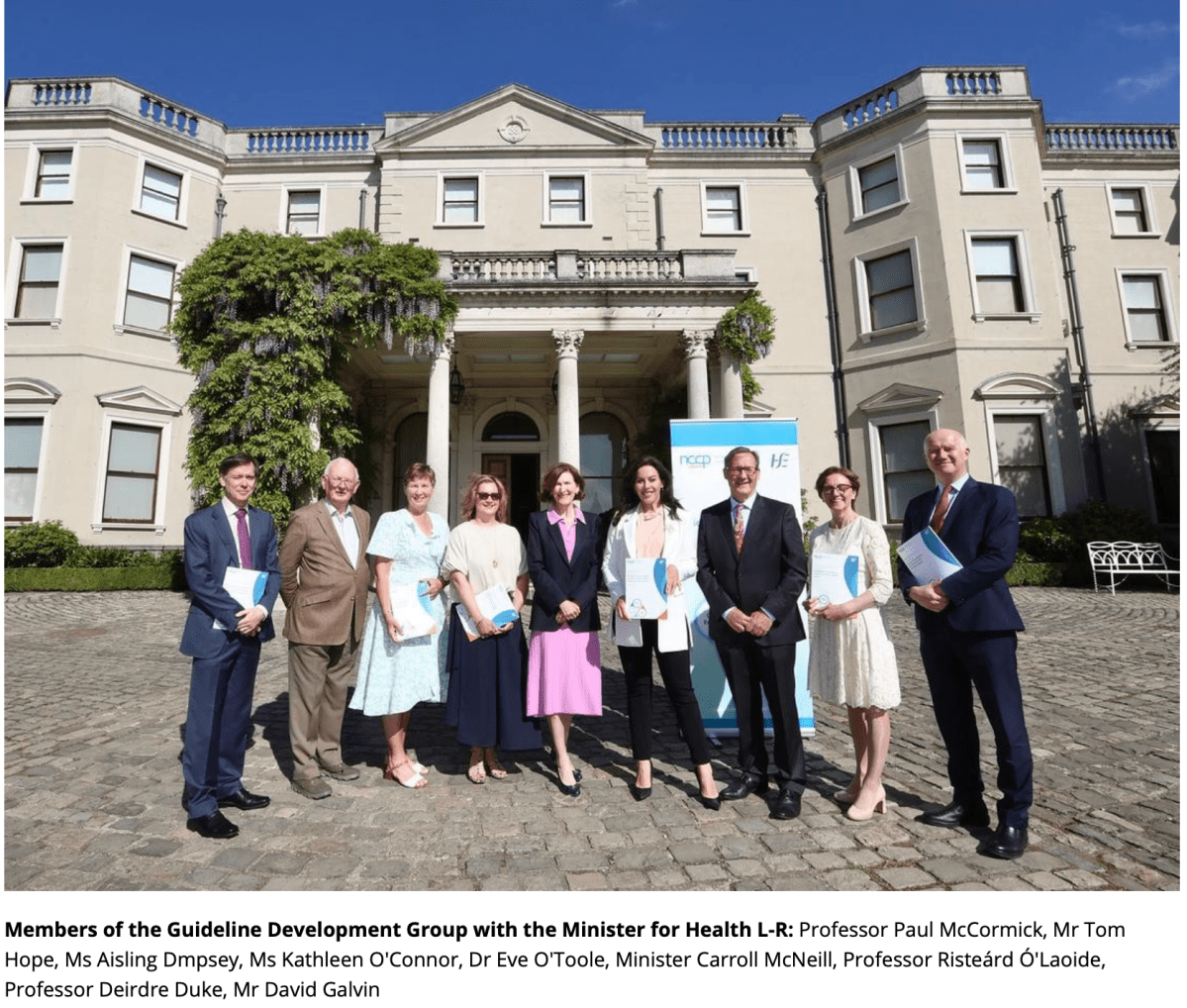
The previous and current National Cancer Strategies recommend that the NCCP develop guidelines for cancer care to improve the quality of care delivered to patients.
To date, nine national clinical guidelines for cancer have been developed, with various updates throughout the years and further updates to continue.
National Clinical Guidelines play a pivotal role in shaping cancer care. They offer patient-centred, evidence-based recommendans that enhance the quality of care provided to patients. They also empower patients to actively participate in decisions relating to their care.
The NCCP recognises the importance of patient input and their role as key stakeholders in developing guidelines. Several patients were invited to contribute to the development of these guidelines which has helped to capture important quality of life issues and patient values.
The guidelines are intended for use by all healthcare professionals involved in multiple stages of the cancer pathway for the three most common cancers in Ireland. They will also be of interest to patients undergoing diagnosis, staging and treatment of these cancers, and their families and carers.