It’s very important to be aware of any changes and let your medical team know about them, even if they happen some time after treatment. There are treatments to help with most side-effects.
Category: Information
Walking a Fine Line as a Squeaky Wheel: Communicating With Doctors
https://raredisease.net/living/communicating-with-doctors
In a nutshell, I walk the line by knowing what my tolerance level is, choosing my battles, and using diplomatic, intentional communication.
Asking a direct question with respect took all the guesswork out of everything for me, and I feel much more secure in our patient-provider relationship.
Number of outpatients seen per consultant has fallen by nearly 30% since 2016
Consultant Medical Oncologist at University Hospital Galway commented on this article to Newstalk FM: https://irishtimes.com/health/2024/07/12/number-of-out-patients-seen-per-consultant-has-fallen-by-nearly-30-per-cent-since-2016/
I am surprised that it is only a 30% reduction. In medical oncology in Ireland, in general, there has never been a ‘waiting list’ to access a consultant opinion, public or private. Since I started my training, every new referral was pretty much automatically booked to the next OPD clinic, i.e. within a week of receiving the referral. That is still the case. 15 years ago, this meant that routinely, a consultant and 2-3 NCHDs would have a 3 hour clinic with 60-70 patients booked in. A patient with a “3pm appointment” would still be waiting to be seen at 8pm. There was little time to discuss the proposed cancer treatment and potential side-effects. The system was clearly understaffed for the volume of patients.
I have said before that one of the positive achievements over the past 10 years is the increase in consultant numbers. This has allowed more meaningful outpatient clinic interactions.
However: If the HSE hires a new consultant with the aim of improving patient care in this way, it should obviously be the case that secretarial support, clinical nurse specialist support, office space, outpatient space, dayward space supported by qualified staff nurses, HSCP support, (theatre space for surgeons), diagnostic and interventional radiology access, etc is also required, to enable improved patient care. In other areas of medicine or surgery, access to a consultant opinion might well be a constraint, in Oncology, the bottleneck is access to the service.
Metaphor
Illness as Metaphor, in her book Susan Sontag sets out to diagnose the problem with the way we think about illness.
Her discovery was not to focus on sickness itself, but the language surrounding disease – language that can, in her view, quite literally kill.
https://www.fringefest.com/festival/whats-on/illness-as-metaphor
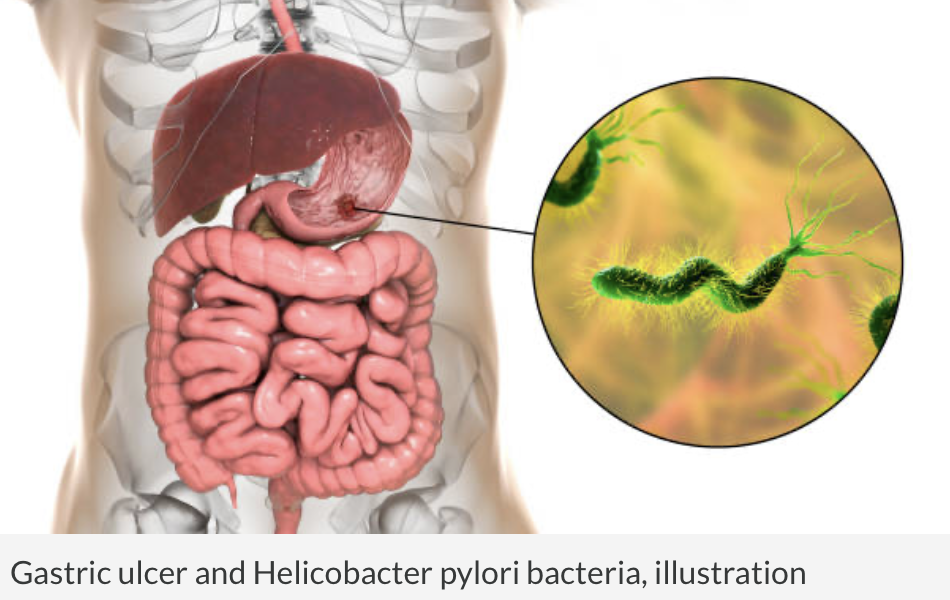
Risk of Gastric and Small Intestinal Cancer in Patients With Lynch syndrome – Data From a Large, Community-Based U.S. Population
This retrospective cohort study included all patients diagnosed with LS between 1/1/1997-12/31/2020 at Kaiser Permanente Northern California. Cumulative incidence of gastric cancer and small intestinal cancer was calculated using competing risk methodology.
Discussion: Patients with LS, particularly MSH2 and MLH1 PV carriers, had significantly increased lifetime risk of gastric and small intestinal cancer. Testing and treatment of H. pylori should be considered for all patients with LS.
Helicobacter pylori (H. pylori) infection occurs when Helicobacter pylori (H. pylori) bacteria infect your stomach. This usually happens during childhood. A common cause of stomach ulcers (peptic ulcers), H. pyloriinfection may be present in more than half the people in the world.
Most people don’t realize they have H. pylori infection because they never get sick from it. H. pylori infection is treated with antibiotics.
Genetic Testing for Hereditary Cancer
Am I required to have genetic testing if I see a genetic counsellor?
No. Genetic counselling involves a detailed evaluation of your family history and family medical records as well as education about hereditary cancer.
Following the initial consultation, some people decide to pursue genetic testing to learn more about the level of cancer risk in their family. Others learn that their family history is not suggestive of an inherited predisposition, or they choose to not pursue genetic testing at this time. These families can still benefit from receiving education about cancer risk, as well as personalized cancer screening and prevention guidelines.
Why is genetic counselling an important part of genetic testing?
There are many different genetic tests, so the counsellor will help each person choose the test that is most appropriate based on their family history and type of information they are looking for. Also, genetic tests that are currently available cannot explain the strong history of cancer in many families. It is important to document the family history in detail so we can provide recommendations for early detection or prevention of cancer, even when genetic testing is not informative. Genetic counselling also addresses important aspects of testing, such as the implications and options for the patient and the impact on family members.
What can I do if I learn I have an increased chance of getting cancer?
There are a variety of options available to people who have an increased chance of cancer based on their family history or genetic testing results. These include increased screening or monitoring, chemoprevention – including medications that reduce the chance of cancer – and risk-reducing surgery. For people who have cancer, the results of genetic testing can sometimes affect the treatment plan.
I’ve already had cancer. What can I learn from genetic counselling?
People who have already had cancer may learn about steps they can take to detect or reduce the chance of other cancers. For example, Lynch syndrome can be associated with an increased chance of Endometrial/Colon cancer.
Genetic counselling will also provide information about whether other family members have an increased chance of developing cancer. There are steps they can take to detect cancer early or prevent it from occurring.
What about insurance discrimination and confidentiality?
The Disability Act 2005 prevent insurers from using genetic testing results to discriminate against individuals.
Part 4 of the Disability Act provides safeguards for the use of information obtained from genetic testing. The provisions aim to ensure that people who may be affected by genetic disorders will not be subject to any unreasonable requirements from an employer or an insurance or mortgage provider. The protections provided are in addition to substantial safeguards for the use of personal information contained in the Data Protection Acts.
The safeguards provide that:
- genetic testing may only take place with a person’s consent, in accordance with the Data Protection Acts
- the results of a genetic test can’t be used in relation to insurance, a mortgage, a personal pension or employment
- the person being tested must be made aware of the intended use of the test results and must, as far as possible, be informed about the possible outcomes of the test
- the use of a person’s family history for insurance purposes may be regulated by the Minister after consultation with other relevant Ministers, the Data Protection Commissioner and other interested bodies or groups
Navigating breastfeeding through cancer treatment
Chemotherapy eventually drew to an end my journey as a breastfeeding cancer patient. This made me very sad. I felt that the decision of when I stopped breastfeeding my child had been taken away from me.Although it was a necessary evil, it would have helped to have had a discussion about it with my medical team, or been signposted to services that could help me through the process.
What you need to know
- When treating a new mother, consider the needs of the mother and baby as a whole, including breastfeeding support
- The breastfeeding network drug fact sheet offers advice for breastfeeding in relation to treatments and investigations
- If a mother has recently stopped breastfeeding, check that any medications you prescribe do not promote lactation
- When might you create a plan to support a mother to continue breastfeeding throughout her treatment or hospital stay?
- What information or resources could you share?
- How could you support a mother who has to be separated from her baby during treatment?
https://www.bmj.com/content/386/bmj.q1284
Sugar-free diets, high dose vitamin C and other false cures for cancer – an expert guide to spotting misinformation
As social media has become less regulated in recent years, and the influence of conspiracy theorists has grown, cancer misinformation has grown along with it. Here is how you can find trustworthy sources….
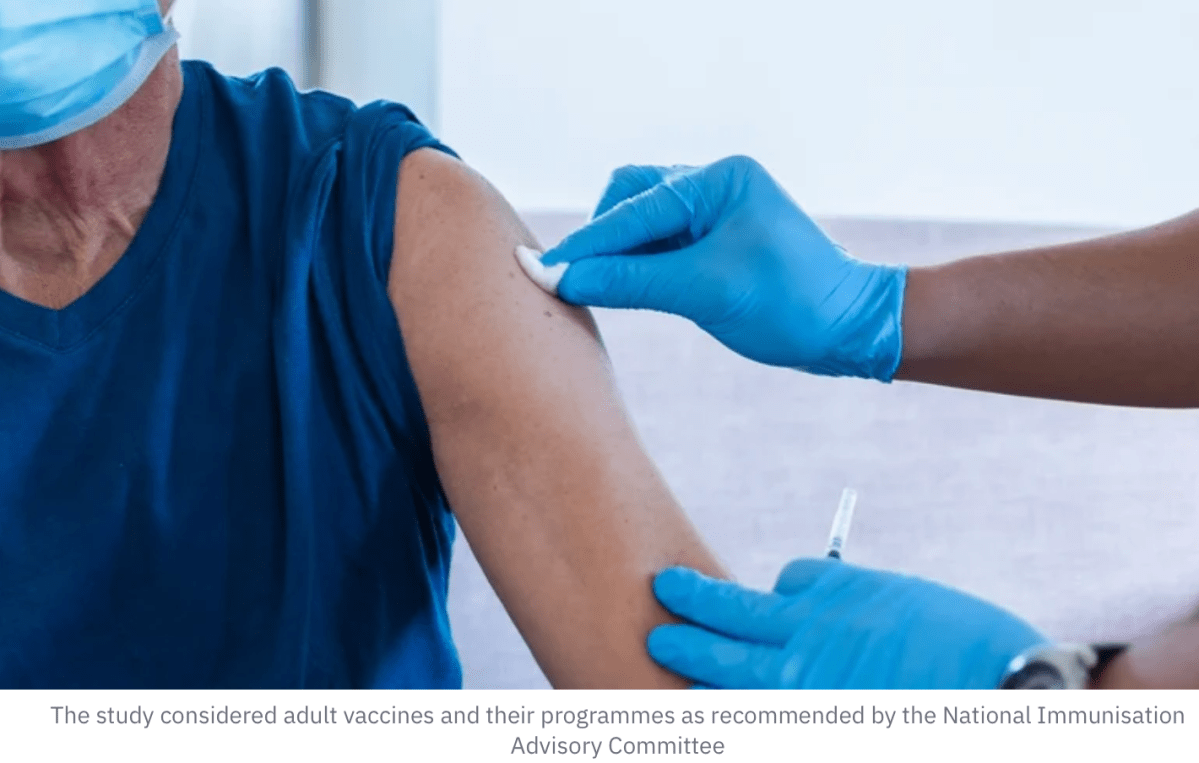
Four vaccine schemes could prevent 1,400 deaths – report
https://www.rte.ie/news/2024/0703/1457891-adult-vaccination-programmes/
A shingles vaccine is available on the market, but it is not given routinely in Ireland.
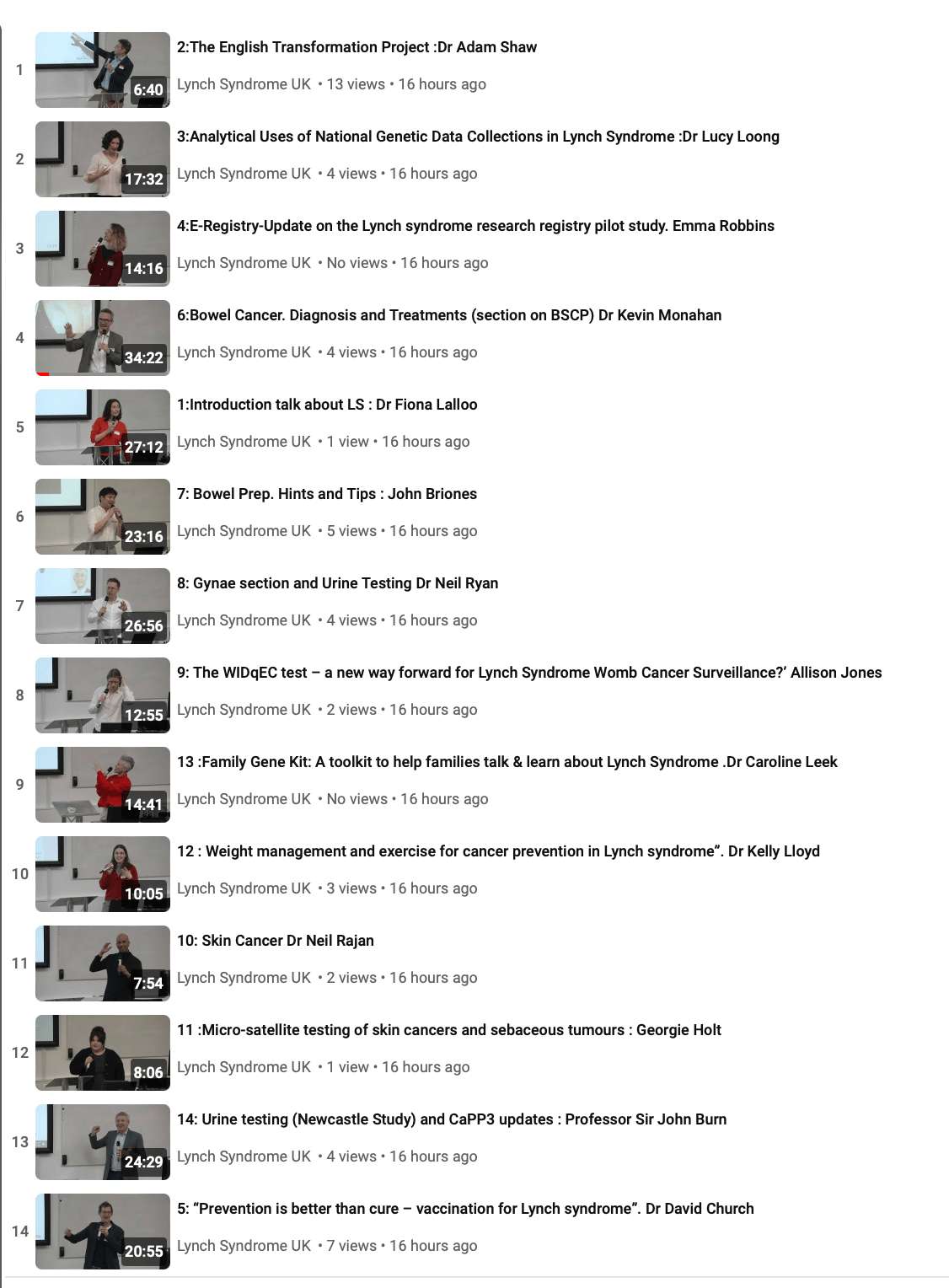
Lynch Syndrome Conference 2024
Check out the presentations on YouTube.
Up to date information on Lynch Syndrome