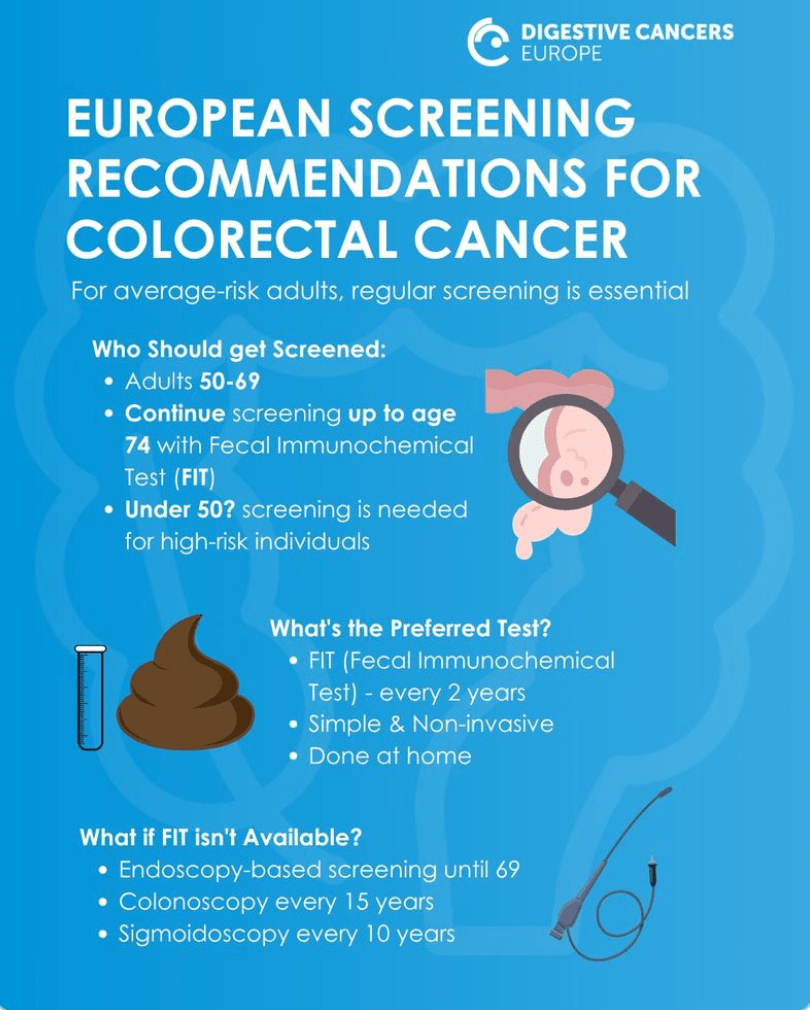
The European Commission’s Joint Research Centre (JRC) has just published updated recommendations on colorectal cancer screening tests and strategies for getting people to participate in screening.
Category: Screening
A Beginner’s Guide to Lynch Syndrome
Lynch Syndrome UK (mob App)
A dedicated Lynch Syndrome app for carriers of LS co-developed by LS UK.
Carriers of this condition can often struggle to access timely information advice.
This digital aid can be helpful to participate directly to prevent complications and personalise their health and well-being plans.
Lynch Syndrome – Cascade Testing
Cascade testing refers to testing “at-risk” family members for a gene mutation, once the mutation has been found in a family member.
For Lynch syndrome, once family members get cascade testing, they can also benefit from screening, cancer prevention, and early detection strategies.
So if a family member has Lynch syndrome
You can ask your GP to refer you to a cancer genetics service.
Family members who can get a test include:
- parents
- brothers or sisters
- children age 18 and over
Ask your relative for a copy of their Lynch syndrome test result or a letter you can bring to your GP appointment – if they have one.
If you get a Lynch syndrome diagnosis, your relatives can ask their GP to refer them to a cancer genetics service. This is known as cascade testing. It is also known as predictive testing.
Lynch syndrome test results can help your healthcare team:
- understand your and your family’s risk of developing cancer in the future
- make a plan to help reduce your risk of cancer
Clinical referral to the NHS following multi-cancer early detection test results from the NHS-Galleri trial
The large, randomised, controlled NHS-Galleri trial (NCT05611632) is assessing the clinical utility of a multi-cancer early detection (MCED) test for asymptomatic cancer screening in England.
Conclusions: To our knowledge, the NHS-Galleri trial has established the first model for the standardised clinical referral of asymptomatic individuals from a trial into NHS standard-of-care cancer pathways. We hope insights from our work could help accelerate screening trial conduct in the UK, and support MCED population screening programme implementation in future.
https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1511816/full
The Myth that Cervical Screening Checks for All Gynecological Cancers
Research in Ireland commissioned by the Irish Network of Gynaecological Oncology (INGO) and supported by Breakthrough Cancer Research highlights the misconceptions that exist surrounding cervical screening, showing that one in three women in Ireland (34%) mistakenly believe that cervical screening checks for all five gynecological cancers
(https://isgo.ie/ingo-outputs/).
Comparison of Universal Genetic Testing vs Guideline-Directed Targeted Testing for Patients With Hereditary Cancer Syndrome
Hereditary factors play a key role in the risk of developing several cancers. Identification of a germline predisposition can have important implications for treatment decisions, risk-reducing interventions, cancer screening, and germline testing.
Key Points:
Questions Does universal genetic testing in patients with cancer identify more inherited cancer predisposition variants than a guideline-based approach, and what is the association between universal genetic testing and clinical management?
Findings In this multicenter cohort study of 2984 patients with cancer, 1 in 8 patients had a pathogenic germline variant, half of which would not have been detected using a guideline-based approach. Nearly 30% of patients with a high-penetrance variant had modifications in their treatment based on the finding.
Meaning Universal genetic testing detected more clinically actionable variants than a guideline-based approach, with a significant association with clinical management for the patients and their families.
https://jamanetwork.com/journals/jamaoncology/fullarticle/2772576/
Improving Cancer Outcomes with Better Lynch Syndrome Testing: A Cost-Benefit Study
While testing of colorectal cancer tumours for mismatch repair defects has been recommended for years, the majority of patients with abnormal results do not complete the next steps, including genetic testing.
Completed genetic testing would determine whether a patient had Lynch syndrome (LS), a hereditary marker for a higher-than-average predisposition for developing colorectal cancer as well as other cancers, including endometrial and ovarian. Early identification of LS in a patient’s family members has the potential to reduce their cancer risk and mortality, increasing the medical benefit of and thereby ultimately lowering testing costs, the study found.
Supporting patient pathway though gynaecological cancer
Women themselves may be unaware of the sometimes symptoms or may be too embarrassed to consult a doctor, and there remains a stigma associated with these diagnoses in some quarters. This reticence needs to be overcome and a more positive message developed to improve the prevention, screening, treatment and care of gynaecological cancers so that women throughout Europe have the best chance of survival and quality of life.
Ovarian, uterine, cervix and other gynaecological cancers are among the most common cancers to affect women, but collectively attract less attention than they deserve from the public and policy makers.
WHAT SHOULD YOU ASK THE DOCTOR?
Useful information before, during, and after your meeting with your doctor(s)
Brochure from ENGAGe (The European Network of Gynaecological Cancer Advocacy Groups is an ESGO network of European patient advocacy groups representing all gynaecological cancers)
https://engage.esgo.org/brochures/what-should-you-ask-the-doctor/
Uptake and patient-related outcomes of mainstreaming genetic testing: a systematic review and meta-analysis
Mainstreaming genetic testing refers to genetic testing for cancer susceptibility genes following cancer diagnosis, which is provided by nongenetic health professionals of the cancer-treating team.
Mainstreaming can be used to guide cancer treatment and secondary cancer prevention in the patient and to identify carriers in the family members of patients who test positive through cascade testing. We aimed to assess uptake and patient-reported outcomes of mainstreaming genetic testing.
Conclusion
Mainstreaming genetic testing uptake is associated with high uptake and satisfaction and low decision conflict, regret, and post-test distress. Quality and quantity of evidence across different types of cancers vary significantly.