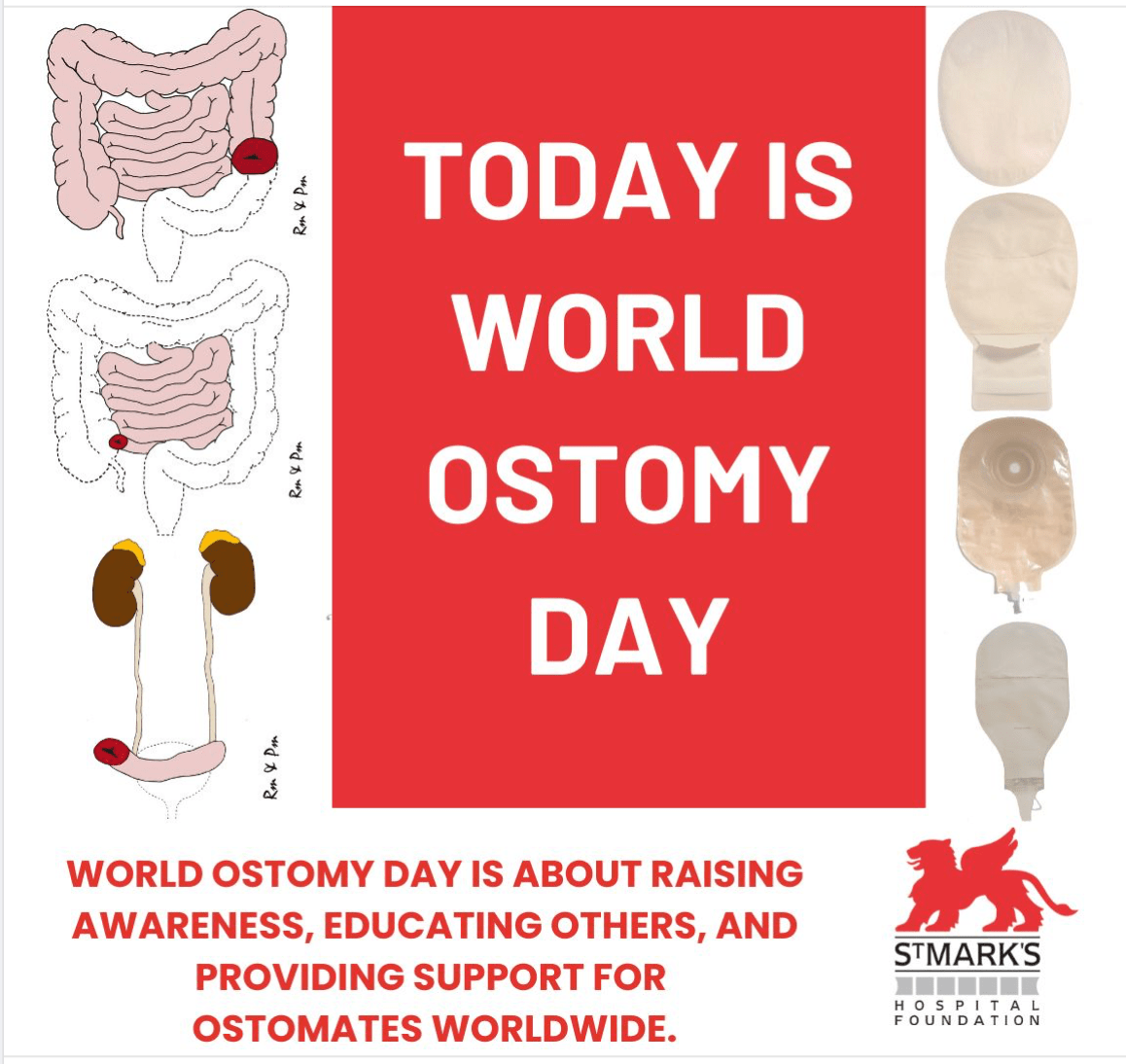
Did you know that 1 in 355 people in the UK live with an ostomy? These numbers represent individuals who show incredible strength, resilience, and determination every single day.
World Ostomy Day is about raising awareness, educating others, and providing support for ostomates worldwide. It’s a chance to celebrate the courage of those who live with an ostomy and to break down stigma. Every story is unique, every journey inspiring!
![]() Help us make a difference:
Help us make a difference:
![]() Share your story or words of encouragement
Share your story or words of encouragement
![]() Raise awareness by talking about ostomies and your experience
Raise awareness by talking about ostomies and your experience
![]() Show support to the ostomy community by using the hashtag #WeAreStMarks and #WorldOstomyDay!
Show support to the ostomy community by using the hashtag #WeAreStMarks and #WorldOstomyDay!