One in Seven Women in Ireland Avoid GP Visits Due to Embarrassment Discussing Symptoms.
- Almost 2,000 Women Diagnosed with Gynaecological Cancers Across Ireland Annually
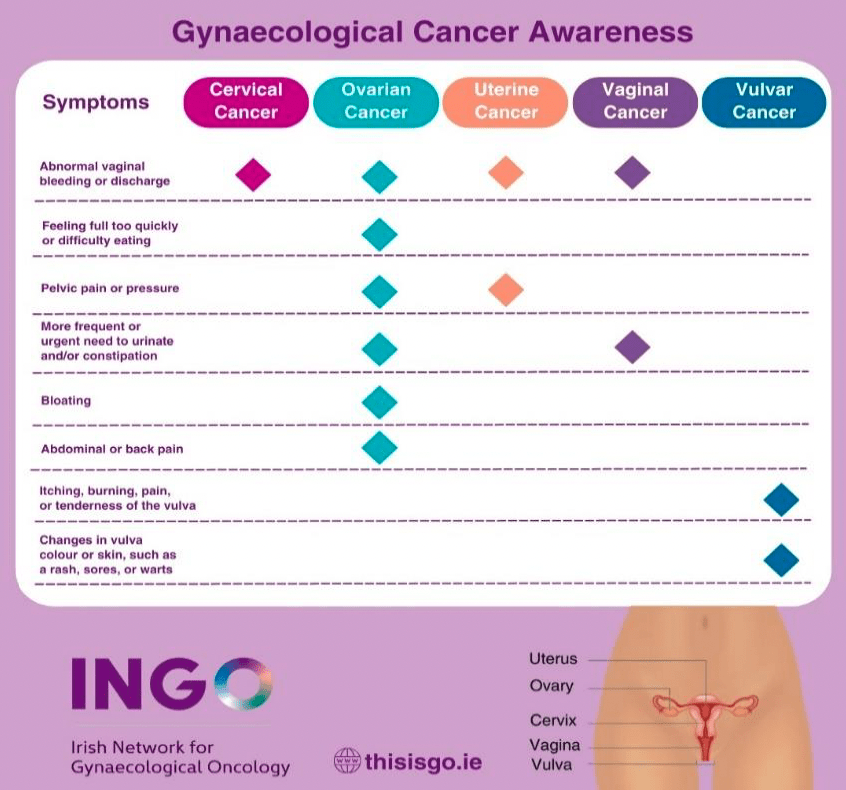
- Only two in five recognise abnormal bleeding or discharge as symptom of uterine cancer
- Only a quarter of women identify changes in urinary habits as symptom of vaginal cancer
Today is World GO Day or World Gynaecologic Oncology Day where patients and advocates around the globe unite to raise awareness about all five gynaecological cancers (vulval, vaginal, cervical, uterine and ovarian) and their risk factors and to combat the stigma associated with gynaecological cancer.
The Irish Network for Gynaecological Oncology (INGO), a voluntary coordination body consisting of over 30 of Ireland’s foremost gynecological cancer campaigners, researchers and patient advocates aim to educate people about the importance of sharing information in relation to prevention, symptoms, early diagnosis and treatment.
Research commissioned by INGO shows that stigma surrounding gynaecological cancers and their symptoms can prevent some women from attending their doctor with warning signs.
One in seven women in Ireland said they would not attend a doctor with cancer warning signs as they find it embarrassing to discuss symptoms, and one in five would not go to the doctor as they do not want to talk to the GP receptionist about symptoms. Furthermore, one in three would not attend if they found it difficult to get an appointment with a particular doctor.
This World GO Day, Fri 20th September, INGO are hosting a free webinar at 1pm for anyone who would like to learn more about the five gynaecological cancers and their symptoms, with insights from cancer patients and medical professionals.
Register for the webinar at http://www.bit.ly/GO_symptoms
http://www.isgo.ie/irish-network-for-gynaecological-oncology/
#WorldGODay2024