2019: A systematic review of 10 189 publications was undertaken to develop 67 evidence and expert opinion-based recommendations for the management of hereditary CRC risk. Ten research recommendations are also prioritised to inform clinical management of people at hereditary CRC risk.
Objective:
To provide a clear strategy for the management of people at hereditary risk of colorectal cancer (CRC), which includes diagnosis, endoscopic management, prevention and surgical care.
Lynch syndrome (LS)
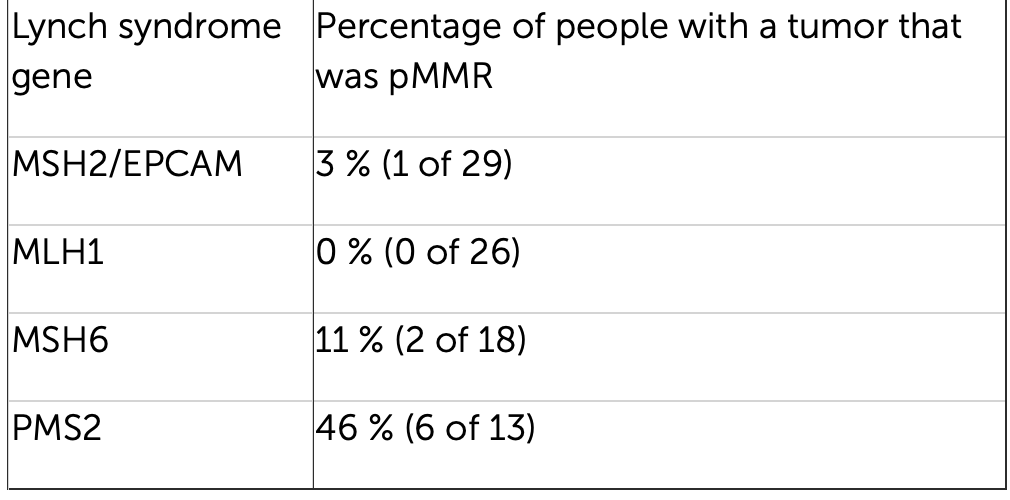
- We recommend that for all people when first diagnosed with CRC, testing using immunohistochemistry (IHC) for MMR proteins or microsatellite instability is used to identify tumours with deficient DNA MMR, and to guide further sequential testing for LS. (GRADE of evidence: moderate; Strength of recommendation: strong)
- We recommend that colonoscopic surveillance should be performed at a 2 yearly interval for all LS patients. (GRADE of evidence: moderate; Strength of recommendation: strong)
- We recommend that age of onset of surveillance colonoscopy should be stratified according to the LS-associated gene. We recommend colonoscopy from age 25 years for MLH1 and MSH2 mutation carriers and 35 years for MSH6 and PMS2mutation carriers. There are insufficient data to support stratifying age of onset of surveillance by gender. (GRADE of evidence: moderate; Strength of recommendation: strong)
- We suggest that for LS patients with MLH1 or MSH2 mutations who develop colon cancer or colonic neoplasia not amenable to endoscopic control, the decision to perform segmental versus total/near total colectomy should balance the risks of metachronous cancer, the functional consequences of surgery, the patient’s age and patient’s wishes. (GRADE of evidence: Moderate; Strength of recommendation: strong)
- We recommend that for LS patients with MSH6 or PMS2 mutations there is insufficient evidence for oncological benefit of extended colectomy over segmental resection. (GRADE of evidence: low; Strength of recommendation: strong)
- We suggest that when abdominal-perineal excision can be avoided, a standard low anterior resection is a reasonable option to treat rectal cancers in LS patients, even though the residual colon is at high-risk of metachronous neoplasia. (GRADE of evidence: low; Strength of recommendation: weak)
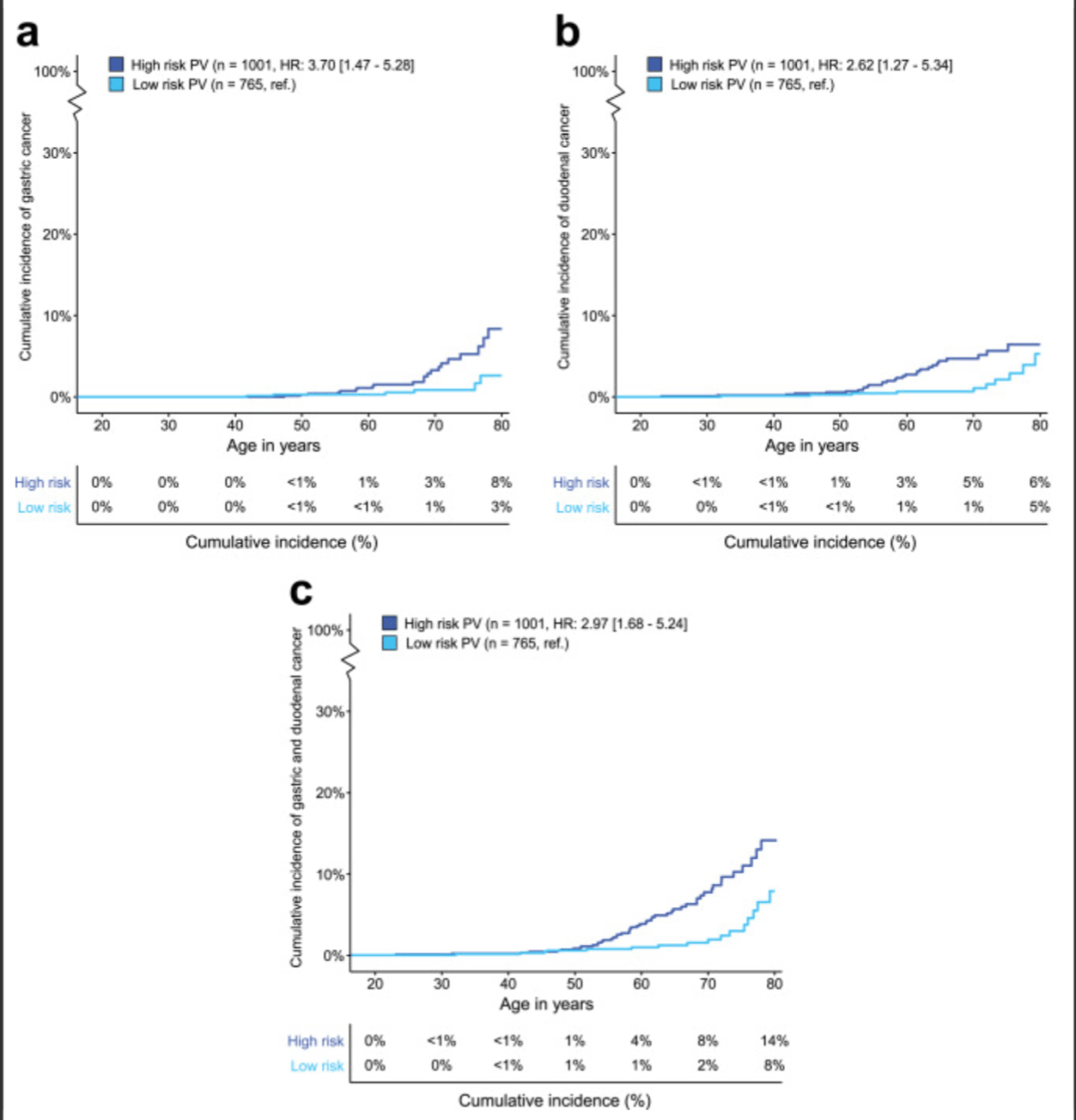
- We recommend that gastric, small bowel, or pancreatic surveillance in LS patients is only performed in the context of a clinical trial. (GRADE of evidence: low; Strength of recommendation: strong)
- We recommend screening for H elicobacter pylori in patients with LS and subsequent eradication therapy if indicated. (GRADE of evidence: low; Strength of recommendation: strong)