GeNotes has been created collaboratively with experts across the NHS to provide practical information and support for fellow clinicians who need to access genomic testing for their patients. Find out more here:
Category: Monitoring
Irish Network of Gynaecological Oncology(INGO)
Congratulations to INGO who was selected as the winner of the Patient Project of the Year Award at the Irish Healthcare Awards 2024 for it’s commitment to raising awareness of gynaecological cancer.
INGO comprises over 30 of Ireland’s foremost gynaecological cancer campaigners, researchers and patient advocates(including Lynch Syndrome Ireland).
Check out http://www.thisisGO.ie an online personalised resource for you and yours who have been impacted by a gynaecological cancer.
Understanding Molecular Classifications of Gynecologic Cancers
Endometrial Cancer
Similar to ovarian cancer, there can be genetic causes at the root of an endometrial cancer diagnosis. It is most commonly a condition called Lynch syndrome, which, according to the Centers for Disease Control and Prevention(USA), is a hereditary condition that predisposes people to colon, endometrial and other cancers.
Lynch syndrome-related cancer may have DNA mismatch repair deficiency (dMMR) and microsatellite instability (MSI or MSI-H). dMMR occurs when DNA strands cannot be properly replicated, leading to mutations. These mutations result in MSI-H cancers.
https://www.curetoday.com/view/understanding-molecular-classifications-of-gynecologic-cancers
In an Ideal World: We would have….
- A central point to support people who are affected by Lynch Syndrome or other Genetic Cancer defects.
- An integrated Cancer Genetics service.
- An increased Genetics workforce.
- A Genetics Testing center in Ireland.
- A comprehensive IT system to Manage/Track and generally improve the collection/storage of relevant information.
- Improved awareness by Public and Medics of Genetics.
- A dedicated Pathway for people with a genetic cancer issue.
- Improved support available to help in relaying a diagnosis to the wider family.
- A national BioBank to improve/help research in this area.
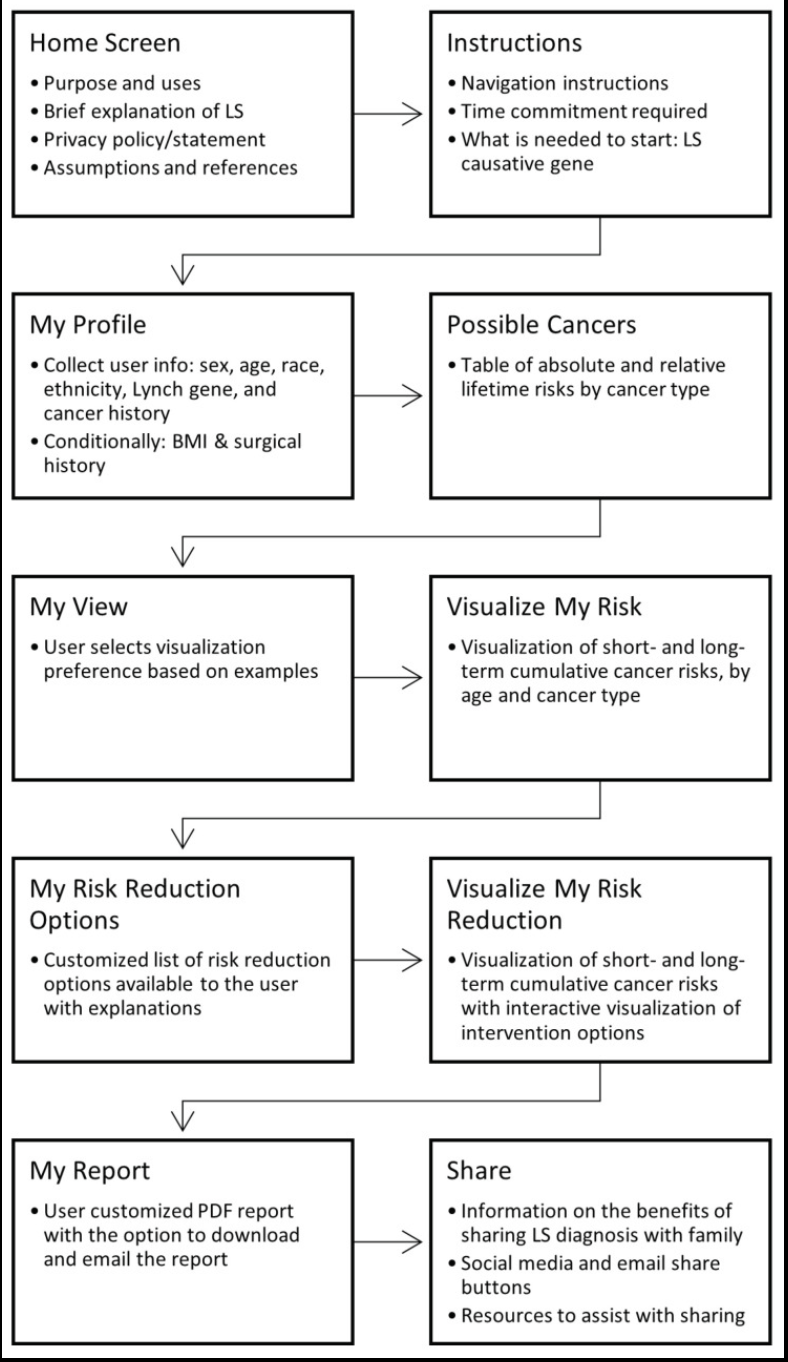
MyLynch: A Patient-Facing Clinical Decision Support Tool for Genetically-Guided Personalized Medicine in Lynch Syndrome (USA)
MyLynch, a patient-facing clinical decision support(CDS) web application that applies genetically-guided personalised medicine(GPM) for individuals with Lynch syndrome.
As genetic panel testing becomes more widely available, GPM will play an increasingly important role in patient care, and CDS tools offer patients and providers tailored information to inform decision-making.
MyLynch provides personalised cancer risk estimates and interventions to lower these risks for patients with LS.
The English National Lynch Syndrome Transformation Project(UK)
Lynch syndrome affects approximately 1 in 400 individuals and predisposes to multiple cancers including colorectal, endometrial, gastric, small bowel and other tumours. Although a common condition, it is estimated that only 5% of patients with LS are known in the UK.
Lifelong care of people diagnosed with this condition depends on awareness of who this population is.
There is consistent evidence of the cost-effectiveness and clinical benefit of a structured diagnostic pathway in patients with LS following a diagnosis of cancer linked to cascade testing in families.
Barriers to diagnosis and a manifest deficiency in care for those with LS has been described in the literature as a ‘diffusion of responsibility’.
An approach to deliver effective diagnosis is to develop ‘mainstreaming’ models whereby patients are offered constitutional genetic testing by their cancer treating teams locally, rather than relying on referral of eligible patients to tertiary services such as clinical genetics.
This has many possible advantages including shorter timescale to diagnosis, effective communication provided through an existing relationship between patients and their clinical teams, and ensuring that eligible patents access testing. This model is associated with high levels of acceptability for patients and clinicians, however relies on the development or new skills by cancer teams.
https://www.bsg.org.uk/clinical-resource/(sss)-english-lynch-syndrome-project
Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG)
2019: A systematic review of 10 189 publications was undertaken to develop 67 evidence and expert opinion-based recommendations for the management of hereditary CRC risk. Ten research recommendations are also prioritised to inform clinical management of people at hereditary CRC risk.
Objective:
To provide a clear strategy for the management of people at hereditary risk of colorectal cancer (CRC), which includes diagnosis, endoscopic management, prevention and surgical care.
Lynch syndrome (LS)
- We recommend that for all people when first diagnosed with CRC, testing using immunohistochemistry (IHC) for MMR proteins or microsatellite instability is used to identify tumours with deficient DNA MMR, and to guide further sequential testing for LS. (GRADE of evidence: moderate; Strength of recommendation: strong)
- We recommend that colonoscopic surveillance should be performed at a 2 yearly interval for all LS patients. (GRADE of evidence: moderate; Strength of recommendation: strong)
- We recommend that age of onset of surveillance colonoscopy should be stratified according to the LS-associated gene. We recommend colonoscopy from age 25 years for MLH1 and MSH2 mutation carriers and 35 years for MSH6 and PMS2mutation carriers. There are insufficient data to support stratifying age of onset of surveillance by gender. (GRADE of evidence: moderate; Strength of recommendation: strong)
- We suggest that for LS patients with MLH1 or MSH2 mutations who develop colon cancer or colonic neoplasia not amenable to endoscopic control, the decision to perform segmental versus total/near total colectomy should balance the risks of metachronous cancer, the functional consequences of surgery, the patient’s age and patient’s wishes. (GRADE of evidence: Moderate; Strength of recommendation: strong)
- We recommend that for LS patients with MSH6 or PMS2 mutations there is insufficient evidence for oncological benefit of extended colectomy over segmental resection. (GRADE of evidence: low; Strength of recommendation: strong)
- We suggest that when abdominal-perineal excision can be avoided, a standard low anterior resection is a reasonable option to treat rectal cancers in LS patients, even though the residual colon is at high-risk of metachronous neoplasia. (GRADE of evidence: low; Strength of recommendation: weak)
- We recommend that gastric, small bowel, or pancreatic surveillance in LS patients is only performed in the context of a clinical trial. (GRADE of evidence: low; Strength of recommendation: strong)
- We recommend screening for H elicobacter pylori in patients with LS and subsequent eradication therapy if indicated. (GRADE of evidence: low; Strength of recommendation: strong)
Worrying won’t change the outcome
It is so important to be vigilant for changes in your body that might be signs of cancer, BUT – it is not your fault if you get cancer, and feeling guilty about not “doing everything right” to prevent it can break people’s souls. @SarahFitzWiMIN
In addition to supports from the Irish Cancer Society and the support of her medical team, Nollaig has found great support through social media. “I came across a Facebook group of women at all different stages of triple negative breast cancer. Rather than reading up on it via Google, you are hearing directly from women who have gone through what you are about to go through. You learn to see that everyone’s experience is different.
Nollaig is sharing her story to raise awareness of breast cancer, but also to call for screening to start at an earlier age.
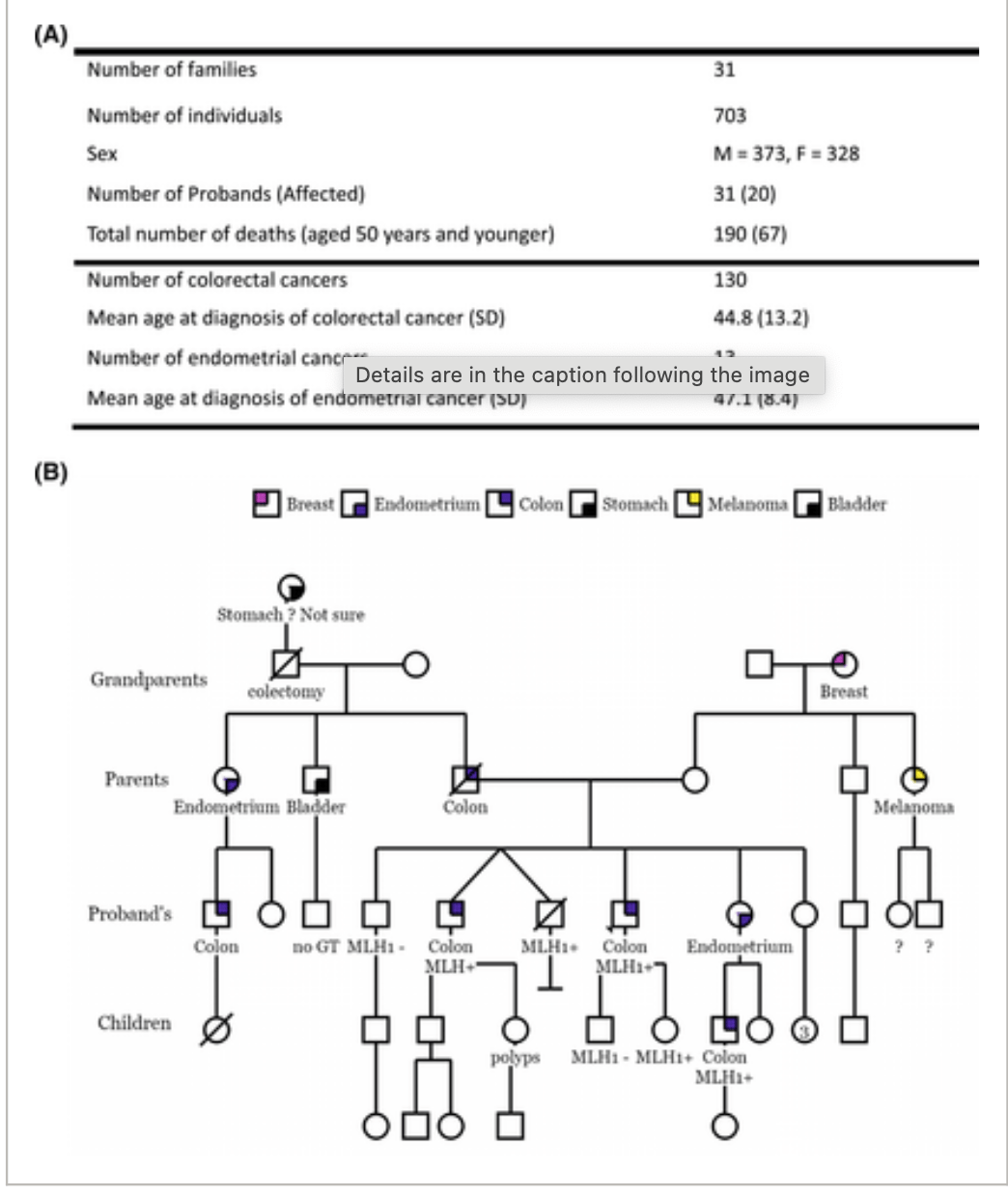
Anticipation in families with MLH1-associated Lynch syndrome
Individuals who have MLH1 PVs have high lifetime risks of colorectal cancer (CRC) and endometrial cancer (EC). There is controversy regarding whether a younger age at diagnosis (or anticipation) occurs in MLH1-associated LS. The objective of this study was to assess anticipation in families with MLH1-associated LS by using statistical models while controlling for potential confounders.
Conclusions
The current results demonstrated evidence in support of anticipation in families with MLH1-associated LS across all statistical models. Mutational effects on Mlh1 activity influenced the hazard for CRC/EC.
https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.35589
Laois rural artist urges people to mind their language on illness
Whether it’s the metaphor of ‘battling cancer’ or the image of ‘frontline workers’ during the pandemic, the author contended that metaphors distort our way of thinking since neither cancer nor Covid are stages of war.
“I have a predisposition to cancer as I carry a gene which is called Lynch Family Syndrome.
“Basically my body cannot detect that cancer is growing in the first place so it very quickly escalates to a grade 4 and because it cannot recognise the disease, it also can’t repair it without help.
“I’m lucky that I know my body well and that I can present myself in time to doctors who have the expertise and modern medicines to reverse the tumour growing.”
“Participating made me look at the psychological effect years after diagnosis. Themes of loneliness, isolation, fear, self-blame, anger and disassociation were explored.