Cancer patients, especially those who are receiving chemotherapy, have a much higher risk of DVT than other people.
Category: Uncategorized
Variant of Uncertain Significance (abbreviated VUS)
When a person undergoes a genetic test it can identify a variant(change), but it is unclear whether that variant is actually connected to a health condition for example Lynch Syndrome.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2825808
Conclusions and Relevance In this cohort study of individuals undergoing genetic testing, the empirically estimated accuracy of pathogenic, likely pathogenic, benign, and likely benign classifications exceeded the certainty thresholds set by current variant classification guidelines, suggesting the need to reevaluate definitions of these classifications.
The relative contribution of various strategies to resolve VUS, including emerging machine learning–based computational methods, RNA analysis, and cascade family testing, provides useful insights that can be applied toward further improving VC methods, reducing the rate of VUS, and generating more definitive results for patients.
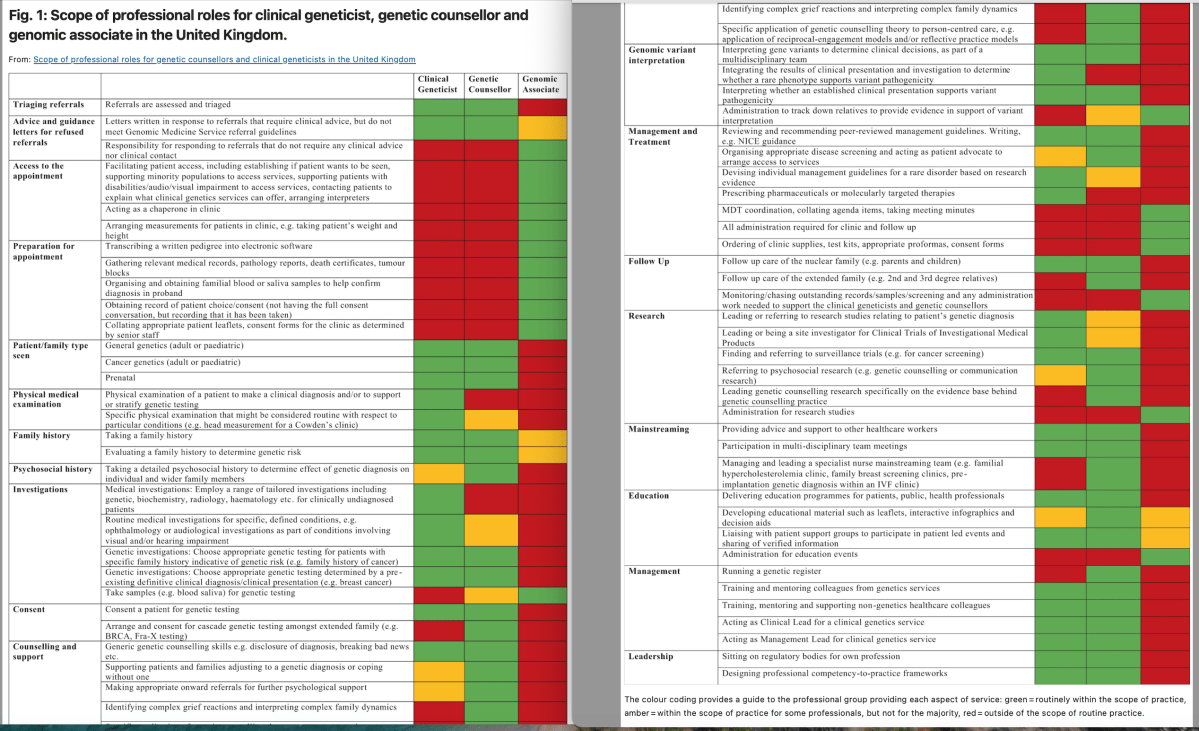
The role of the Genetic Counsellor in the multidisciplinary team: the perception of geneticists in Europe(2022)
Genetics has begun to be considered a key medical discipline which can have an impact on everyday clinical practice. Therefore, it is necessary to understand what the most effective way is of caring for people affected by or at risk of genetic disorders.
This new profession has difficulties in being recognised in some countries(including Ireland), it seems clear that these highly competent professionals are essential for in-patient care and in the multidisciplinary team.
In the United Kingdom clinical geneticists are medically qualified Members/Fellows of the Royal College Physicians or equivalent, where Clinical Genetics is an affiliated medical specialty. Genomic or genetic counsellors are allied health professionals with Masters level accreditation from the Genetic Counsellor Registration Board included in the Academy for Healthcare Science register and clinical scientists (genomic counselling specialty) accredited by the Health and Care Professions Council. https://www.nature.com/articles/s41431-022-01214-7/figures/1
This research(although limited) brought to light the importance of the multidisciplinary team in caring for patients with or at risk of genetic disorders by highlighting the role and necessity of the genetic counsellor within the team.
https://www.nature.com/articles/s41431-022-01189-5?fromPaywallRec=false
‘A day of hope’: Irish hospital patients get access to ‘early phase’ cancer drugs
“Today is a day of hope,” said Mater hospital chairman David Begg as it launched an initiative which could mean cancer patients securing access to cutting-edge drug treatments in the State years in advance of when this would otherwise have been the case.
Miriam….“While I did not have the benefit of a clinical trial, I have received new treatments that have come through in the last six to seven years. I am currently stable [but] I have had the last line of treatment. So I am looking for what is coming next.”
Hope you are having a good day
Individual Health Identifier (IHI)
Did you know….
The Health Identifiers Act 2014 was enacted by the government to allow two new national data collections–called the National Register of Individual Health Identifiers and the National Register of Health Service Provider Identifiers to be created and operated.
An Individual Health Identifier (IHI) has the following benefits for you:
Improved accuracy in identifying you and your medical records will
lead to safer and better care being provided to you.
Improved accuracy in identifying and associating your records in
different healthcare organisations.
Your health information can be shared safely and seamlessly
between health service providers, for example on referral letters
sent from a private GP to a public hospital.
The use of an Individual Health identifier also enables the
electronic transfer of your health information, which results in faster
care for you.
Medical or clinical information will NEVER be stored on your IHI record. Health
service providers may however use your IHI, to uniquely identify you, when
communicating with other health service providers about your care for example
when a medical consultant is corresponding with your GP or visa versa.
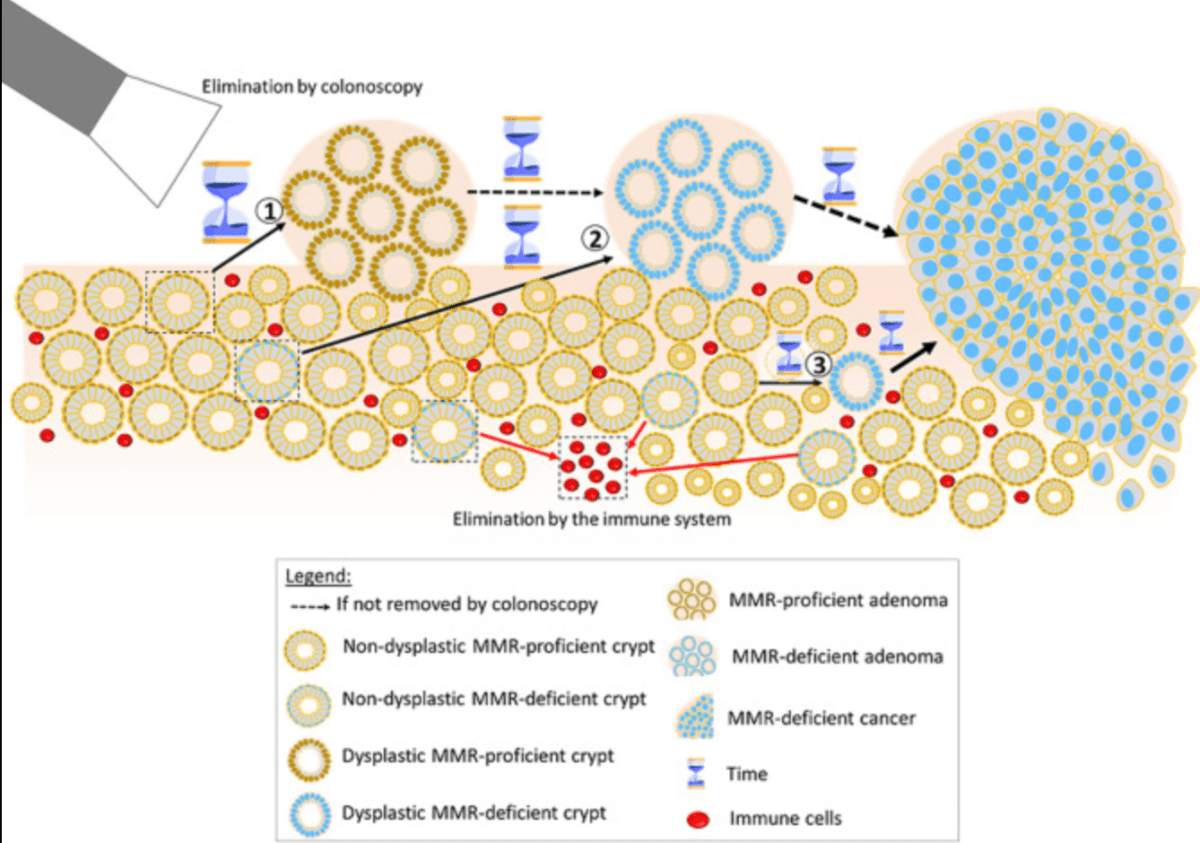
Incidences of colorectal adenomas and cancers under colonoscopy surveillance suggest an accelerated “Big Bang” pathway to CRC in three of the four Lynch syndromes
Conclusions: Colonoscopy prevented CRC in path_PMS2 carriers but not in the others. Our findings are consistent with colonoscopy surveillance blocking the adenoma-carcinoma pathway by removing identified adenomas which might otherwise become CRCs. However, in the other carriers most CRCs likely arised from dMMR cells in the crypts that have an increased mutation rate with increased stochastic chaotic probabilities for mutations. Therefore, this mechanism, that may be associated with no or only a short sojourn time of MSI tumours as adenomas, could explain the findings in our previous and current reports.
path_MMR:Pathogenic or likely pathogenic variant in one of the MMR genes (MLH1, MSH2, MSH6, or PMS2)
https://pubmed.ncbi.nlm.nih.gov/38741120/
Overall….colonoscopy works either by preventing some cancer, or where this is not biologically possible- by diagnosing cancer early.
[GDPR] is being used in Ireland as a reason not to do things, as an excuse not to share data
Where do non-invasive colorectal cancer tools ‘FIT’ alongside colonoscopy in the surveillance of high-risk patients?
There is increasing interest in the use of less-invasive approaches to investigation of at-risk populations, driven in part by the COVID19 pandemic as resources have been increasingly constrained, alongside expanding evidence of clinical effectiveness.
Fecal hemaglobin immunochemical testing(FIT) has been validated in screening and symptomatic populations, is cost-effective, and acceptable to patients.
As a quantitative assay, lower fHb concentration thresholds increase CRC sensitivity albeit with decreased specificity, however FIT has a lower sensitivity for advanced adenomas of around 40-60%2. Therefore a ‘FIT only’ strategy may theoretically result in fewer prevented CRCs, notwithstanding a limited understanding of the natural history of familial CRC. However the estimated reduction in risk by removal of precursor advanced adenomas at colonoscopy provides an opportunity for a less-invasive combined strategy using FIT.
In conclusion the authors have developed a compelling rationale for a combined FIT:colonoscopy strategy where previous data has indicated that FIT alone would not be sufficient. Although their study did not identify differences according to levels of CRC risk, further refinement of risk estimates and investigative strategies may facilitate risk-stratified mixed-modality surveillance strategies.
https://www.gastrojournal.org/article/S0016-5085(24)05458-1/pdf
Ciara shares how knowledge of her Lynch Syndrome status enabled her to avail of risk-reduction measures that prevented endometrial cancer
We wish to thank Ciara for allowing us to share her story for World Gynaecological Oncology Day. Ciara hopes by sharing her story she can raise awareness of the role genetic risk-factors play in the development of gynea cancers and give hope to others 💜
Over the years, I was aware of Lynch syndrome due to several members of my Mum’s family having it. My great aunt had wrote out a family tree of all family with the inherited gene. That valuable information was then transferred to the genetics clinic.
After a blood sample in 2017, the genetics clinic confirmed that I had Lynch Syndrome with MSH2 gene alteration. It was recommended that I go for a colonoscopy every two years.
Two years ago I was referred to the Gynaecology department for surveillance. Blood tests, ultrasound tests and endometrial biopsies were offered. It was then I started to research the lifetime risk of endometrial cancer associated to MSH2 (40-60%) and understand the importance of surveillance. My endometrial biopsy confirmed I had atypical endometrial hyperplasia which is a pre-cancerous condition of the uterus. Having risk reducing surgery at 44 was the only and logical thing to do my situation. It has been a lot to process emotionally at times, but I am fortunate to have a loving partner, friends, family and other outlets for support. Under the exceptional care of Dr Astbury and her team at UHG, I had a full abdominal hysterectomy in February this year and have recovered well. I am very lucky the endometrial biopsy surveillance was done when it was. The early detection prevented me from needing further treatment after my surgery. I will be forever grateful for everything Dr Astbury and her team have done in order to protect my health.
Ciara Donoghue
#WorldGODay2024 #GynaeCancers #riskfactors #earlydetection #HereditaryCancers #CancerGenetics