Once a medicine has been approved at a European level, the pharmaceutical company will make separate applications for reimbursement at a national level in different EU or EEA countries. In Ireland these applications are made to the HSE Corporate Pharmaceutical Unit (CPU) who then commission the National Centre for Pharmacoeconomics (NCPE) to carry out an assessment on that medicine.
A full health technology assessment (HTA) is a systematic assessment of the clinical and cost-effectiveness of a medicine. Only a selection of medicines are required to undergo a full HTA as part of the drug reimbursement process. The NCPE full HTA assessment takes approximately 18 weeks to complete, exclusive of the duration the HTA is queried with the Applicant (approximately five weeks as part of the stop/clock process). The full HTA report consists of the following information:
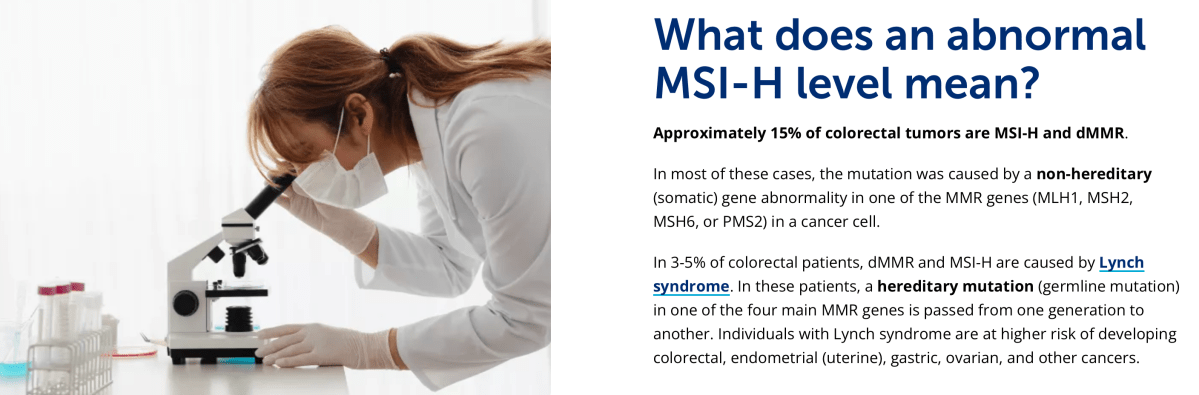
- Disease background and epidemiology
- Detailed description of current clinical practice and treatment options
- Detailed description of the intervention (drug) under assessment
- Detailed review of the clinical and comparative efficacy of the drug under assessment
- Detailed review of the safety and comparative safety of the drug under assessment
- Detailed review of the cost-effectiveness of the drug under assessment
- Detailed review of the budget impact of the drug under assessment.
The outcome of a full HTA is a recommendation to the HSE on reimbursement.
I’m confused…
Do public cancer patients have the same chance of living as those with health insurance? It appears you have across all cancers a better, faster access to cutting-edge drugs in the private system compared to the public system
Are pharmaceutical companies making separate applications for reimbursement at a national level in a timely manner? If so why is this?
Is NCPE adhering to its own time frames? If not why?
It appears that up to 40% of the new medicines approved by the EMA are not even assessed by the HSE because its approval system is so protracted it can sometimes take up to three years for the health authority to decide whether to provide the drug free of charge.Is this a process being used to slow down the approval of new drugs to save money?
Who is actually in Charge of spending the Taxpayers money?????