Many men with cancer in the family worry that they are at greater risk of getting it themselves. But this isn’t the case for most people. Cancer is a common disease among older people, so most families will include at least one person who has had cancer.
The more relatives who have had cancer, and the younger they were at diagnosis, the stronger your family history. You may have a strong family history if any of these situations apply to you:
- More than two close relatives on the same side of your family have had cancer.
- The cancers developed when they were young (under the age of 50).
- One of your relatives has had a gene fault found by genetic tests.
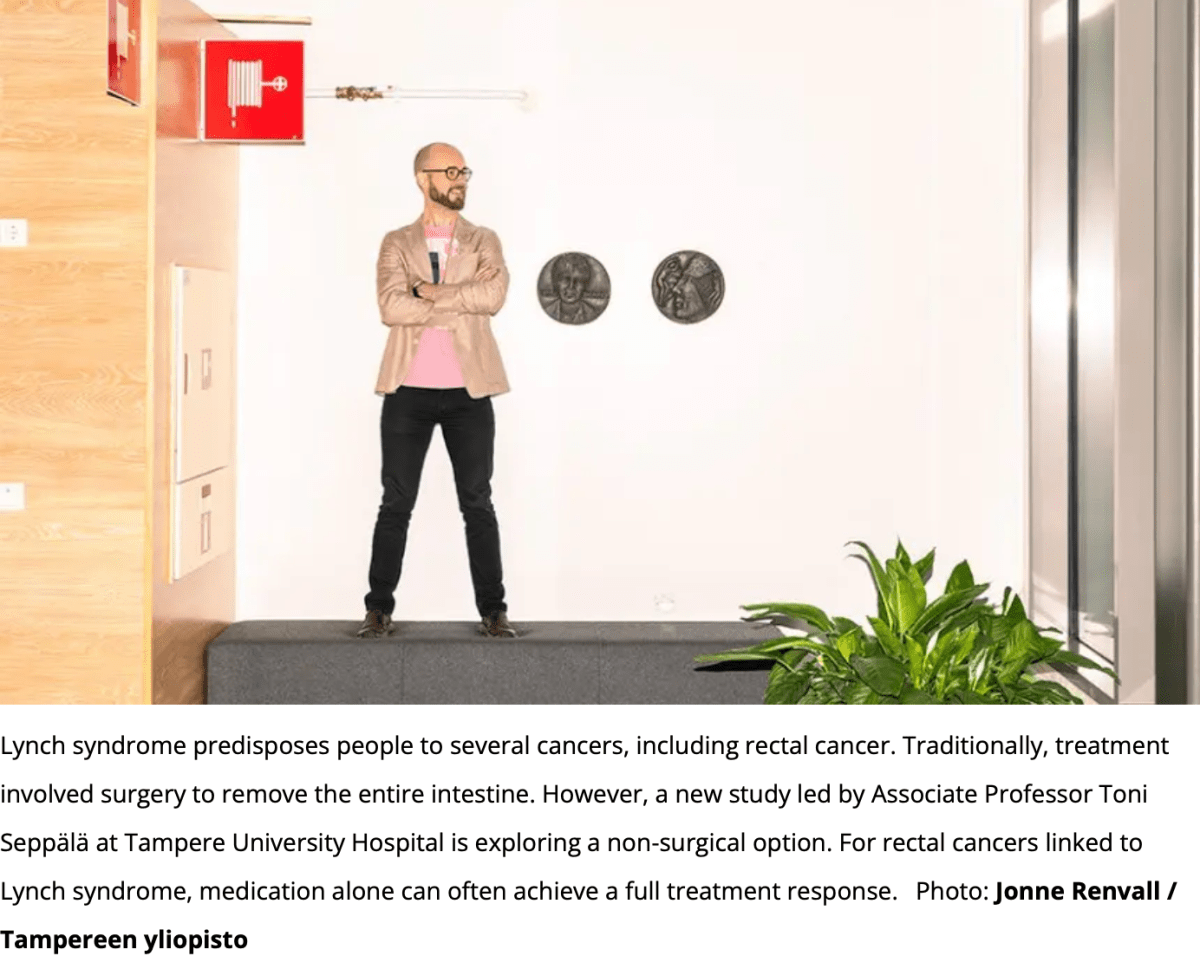
5 – 10% of cancers are linked to an inherited gene fault.
What should I do if I have a family history of cancer?
Talk to your doctor who can help you find out if your family history of cancer is of concern. Your doctor may suggest that you visit regularly for screening. In this way, you can pick up problems early.