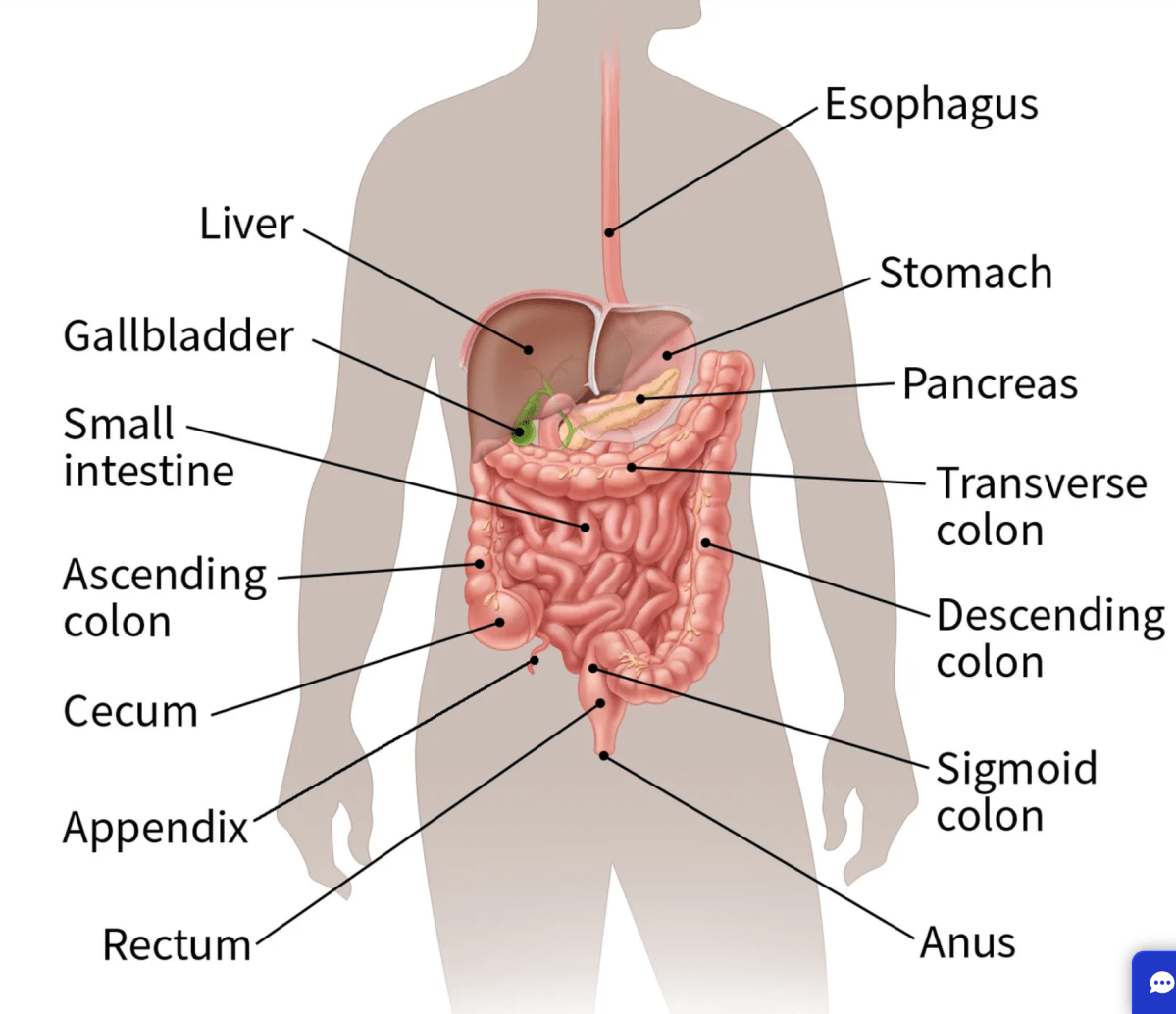
Lynch syndrome affects approximately 1 in 400 individuals and predisposes to multiple cancers including colorectal, endometrial, gastric, small bowel and other tumours. Although a common condition, it is estimated that only 5% of patients with LS are known in the UK.
Lifelong care of people diagnosed with this condition depends on awareness of who this population is.
There is consistent evidence of the cost-effectiveness and clinical benefit of a structured diagnostic pathway in patients with LS following a diagnosis of cancer linked to cascade testing in families.
Barriers to diagnosis and a manifest deficiency in care for those with LS has been described in the literature as a ‘diffusion of responsibility’.
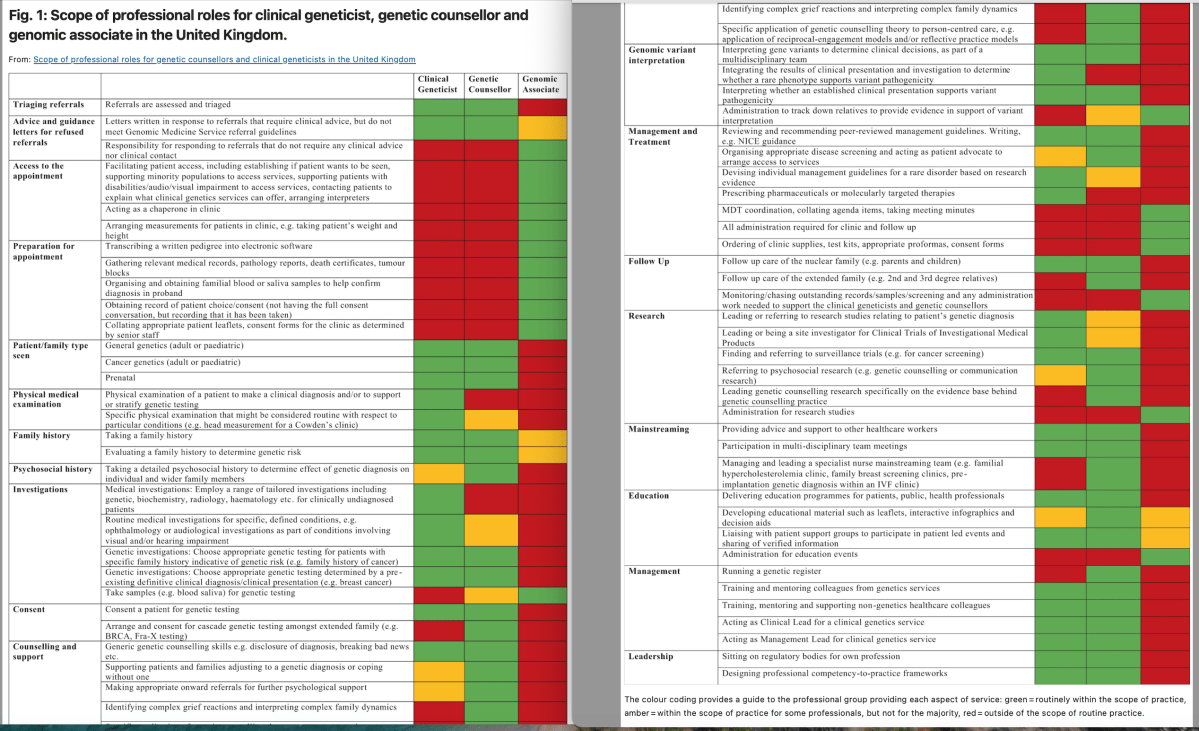
An approach to deliver effective diagnosis is to develop ‘mainstreaming’ models whereby patients are offered constitutional genetic testing by their cancer treating teams locally, rather than relying on referral of eligible patients to tertiary services such as clinical genetics.
This has many possible advantages including shorter timescale to diagnosis, effective communication provided through an existing relationship between patients and their clinical teams, and ensuring that eligible patents access testing. This model is associated with high levels of acceptability for patients and clinicians, however relies on the development or new skills by cancer teams.
https://www.bsg.org.uk/clinical-resource/(sss)-english-lynch-syndrome-project